An experimental vaccine to prevent the mosquito-borne viral illness chikungunya elicited neutralizing antibodies in all 25 adult volunteers who participated in a recent early-stage clinical trial conducted by researchers at the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health.
The most distinctive symptom of chikungunya infection is severe joint pain accompanied by headache and fever. There are currently no vaccines or specific drug treatments for chikungunya. First identified in East Africa in the early 1950s, chikungunya virus caused sporadic illness in Africa and large urban outbreaks in Thailand and India in the 1960s and 1970s. It first appeared in the Western Hemisphere in late 2013.
As of August 8, more than 570,000 confirmed or suspected cases had been reported throughout the Americas. In the continental United States, 484 cases have been reported as of August 5, and the first two locally acquired infections were detected in Florida in mid-July.
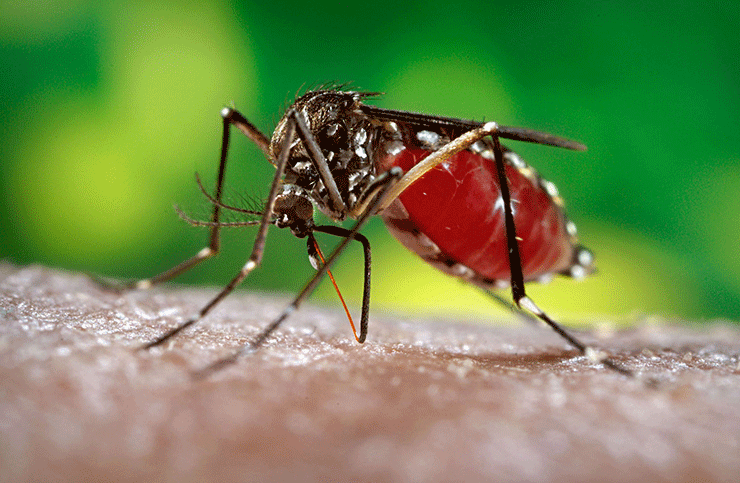
“The two species of mosquito that spread chikungunya virus are found in parts of the continental United States, so it may just be a matter of time before this illness gains a foothold here,” said NIAID Director Anthony S. Fauci, M.D. “Therefore, it is prudent to begin addressing this emerging public health threat with the development of vaccines, such as this one, which was designed and tested by scientists from the NIAID Vaccine Research Center.”
In 2010, Vaccine Research Center (VRC) scientists and colleagues tested this candidate chikungunya vaccine in non-human primates. All of the immunized animals were protected from infection when later exposed to chikungunya virus.
In the newly reported trial, 23 healthy volunteers received three injections (two other volunteers received two injections) of vaccine at one of three different dosages (10, 20 or 40 micrograms) over a 20-week span. Antibody production was measured at multiple time points following each injection. Investigators detected chikungunya neutralizing antibodies in all volunteers following the second injection, with a significant boost of neutralizing antibodies seen following the third injection. Vaccine-induced antibodies persisted in all volunteers, even those who received the lowest dosage, for at least 11 months after the final vaccination, suggesting that the vaccine could provide durable protection against disease.
“The candidate vaccine prompted a robust immunological response in recipients and was very well tolerated,” noted VRC scientist Julie E. Ledgerwood, D.O., principal investigator of the trial. “Notably, the levels of neutralizing antibody produced in response to the experimental vaccine were comparable to those seen in two patients who had recovered from a chikungunya virus infection acquired elsewhere. This observation gives us additional confidence that this vaccine would provide as much protection as natural infection.”
Whereas traditional vaccines are typically made from either killed viruses or from weakened live viruses, the experimental vaccine used in the trial is a different type: a virus-like particle (VLP) vaccine. VLP vaccines contain the outer shell proteins of a virus without any of the material the virus needs to replicate inside cells. VLP vaccines often prompt an immune reaction similar to that of natural, whole virus and have a number of potential advantages over traditional vaccines, said Dr. Ledgerwood. Notably, because no live viruses are used in their manufacture, VLP vaccines do not need to be produced under high-level biocontainment conditions.
This candidate vaccine was delivered without an adjuvant — a substance added to vaccines to improve the immune response — but still prompted a good response, said Dr. Ledgerwood. If the candidate were to be formulated with an adjuvant, she added, it might be possible to achieve similar immune responses at lower vaccine dosages.
Source: NIH, adapted.