Bold text highlights added by Global Biodefense editors.
James S. Brady Press Briefing Room
4:03 P.M. EST – JANUARY 21, 2021
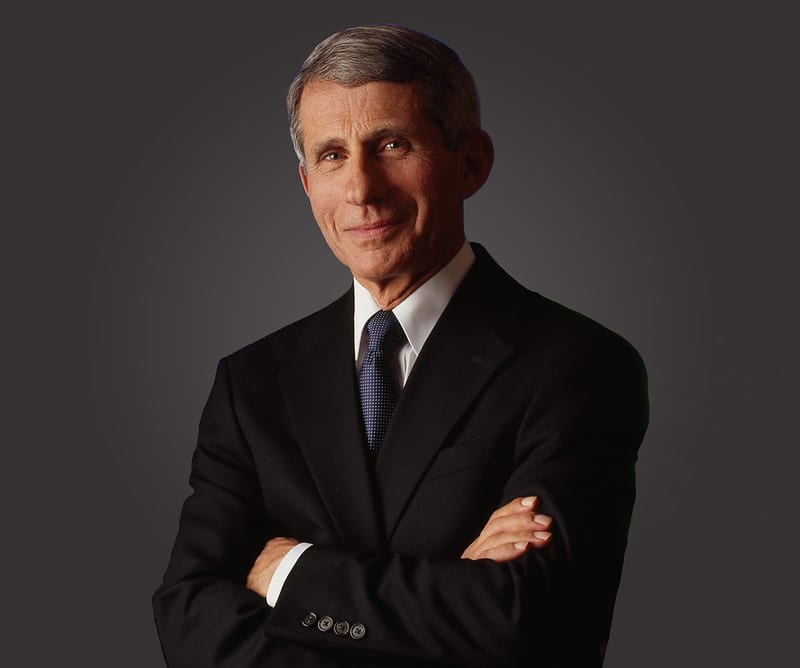
MS. PSAKI: Good afternoon. Thank you for joining us today. Many familiar faces from yesterday back again. We are pleased to have Dr. Fauci here with us as part of the President’s commitment to have public health experts lead our communication with the American people about the pandemic.
Just to give you a bit of a run of show here: Dr. Fauci will speak at the top about the state of the pandemic, the status of vaccines. He’ll take some of your questions. I will play the role of the bad cop when it’s time for him to go and get to the work of the American people. And then I will do a topper, and I’ll answer a bunch of your questions as well.
So, there’s lots to come after this. With that, I will turn it over to Dr. Fauci.
DR. FAUCI: Thank you very much. And I’m going to just spend a couple of minutes just summarizing the status of where we are and then maybe addressing some of the things that I know are on people’s minds.
So, first of all, obviously we are still in a very serious situation. I mean, to have over 400,000 deaths is something that, you know, is, unfortunately, historic in the very — in the very bad sense. When you look at the number of new infections that we have, it’s still at a very, very high rate. Hospitalizations are up. There are certain areas of the country, as I think you’re all familiar with, which are really stressed from the standpoint of beds, from the standpoint of the stress on the healthcare system.
However, when you look more recently at the seven-day average of cases — remember, we were going between 300,000 and 400,000, and 200,000 and 300,000. Right now, it looks like it might actually be plateauing in the sense of turning around.
Now, there’s good news in that, but you have to be careful that we may not be seeing perhaps an artifact — an artifact of the slowing down following the holidays. So when we see that, we think it’s real.
But one of the things — and it’s interesting — I’m, sort of, getting a deja vu standing up here, because I said something like this almost a little bit less than a year ago, when we were talking about the acceleration of cases in the late winter/early spring of 2020, when we were having New York City metropolitan area being the epicenter of what was going on — that there are always lags, so please be aware of that; that when you have cases, and then a couple of weeks later, you’ll see it represented in hospitalizations, intensive care, and then a couple of weeks later, in deaths.
So you have almost paradoxical curves, where you see something plateauing and may be coming down at the same time as hospitalizations and deaths might actually be going up.
So this is something that I just put on your radar screen. It is not an unusual thing to see that sort of thing.
The other point I want to make is one that we’re getting asked a lot regarding questions, and that is: What is it about these mutants that you’re hearing about — the mutants in the UK, which we know are in about 20-plus states; the mutants that we’re seeing in South Africa and in Brazil?
First of all, we need to understand that RNA viruses, like coronaviruses, mutate all the time. Most of the mutations don’t have any physiological relevance with regard to the function of the virus itself. However, every once in a while, you get mutations, either singly or clustered in combinations, which do have an impact.
So what have we learned thus far? And I want to emphasize “thus far” because we’re paying very, very careful attention to this, and we take it very seriously. At least from the experience that our colleagues in the UK have had, the one that is in the UK appears to have a greater degree of transmissibility — about twice as much as what we call the “wild type” original virus. The one that is in South Africa is a bit different, and I’ll get to that in a second.
So it does look like it increases the transmissibility. They say, correctly, on a one-to-one basis, it doesn’t seem to make the virus more virulent or have a greater chance of making you seriously ill or killing you. However, we shouldn’t be lulled into complacency about that, because if you have a virus that is more transmissible, you’re going to get more cases. When you get more cases, you’re going to get more hospitalizations. And when you get more hospitalizations, you’re ultimately going to get more deaths. So even though the virus, on a one-to-one basis, isn’t more serious, the phenomenon of a more transmissible virus is something that you take seriously.
The next thing is: Does it change enough to interfere with the efficacy of a whole group of monoclonal antibodies that many of you are aware of? The monoclonal antibodies that are being used for treatment, in some cases, and prevention. Since monoclonal antibodies bind to a very specific part of the virus, when there’s a mutation there, it has much greater chance of obliterating the efficacy of a monoclonal antibody. And we’re seeing in the much more concerning mutations that are in South Africa — and in some respects, Brazil, which is similar to South Africa — that it is having an effect on the monoclonal antibodies.
The real question that people are quite clearly interested in is: What is the impact on the vaccine? And, so far, literally, we have this new phenomenon that a preprint journals, where — where people get data, and they put it into a preprint server where it hasn’t yet been peer reviewed, but you have to pay attention to it because it gives you good information quickly. Ultimately, it gets confirmed.
And we’re seeing them coming out over the last few days, and what they’re saying is that what we likely will be seeing is a diminution — more South Africa than UK — UK — is that diminution in what would be the efficacy of the vaccine-induced antibodies.
Now, that does not mean that the vaccines will not be effective, and let me explain why. There’s a thing called a “cushion effect.” So, if you have a vaccine, like the Moderna and the Pfizer vaccine, that can suppress the virus at a dilution, let’s say, of 1 to 1,000, and the mutant influences it by bringing it down to maybe 1 to 800, or something like that, you’re still well above the line of not being effective. So there’s that “cushion” that even though it’s diminished somewhat, it still is effective. That’s what we’re seeing, both certainly with the UK, which is very minimal effect. We’re following very carefully the one in South Africa, which is a little bit more concerning, but nonetheless, not something that we don’t think that we can handle.
What is the message? Because someone can say, “Now, wait a minute — if you have the possibility that the vaccines are diminishing in their impact, why are we vaccinating people?” No. It is all the more reason why we should be vaccinating as many people as you possibly can. Because as long as the virus is out there replicating — viruses don’t mutate unless they replicate. And if you can suppress that by a very good vaccine campaign, then you could actually avoid this deleterious effect that you might get from the mutations.
Bottom line: We’re paying very close attention to it. There are alternative plans if we ever have to modify the vaccine. That is not something that is a very onerous thing. We can do that given the platforms we have. But right now, from the reports we have — literally, as of today — it appears that the vaccines will still be effective against them, with the caveat in mind you want to pay close attention to it.
So, Jen, why don’t I just stop there and then maybe just answer some questions on anything else that I said?
So, yeah.
Q How helpful would it have been if Amazon got involved with the federal response to COVID-19 before Biden took office? And do you know about any plans or discussions ahead of yesterday?
DR. FAUCI: No, I don’t think I could answer that question. I’d be waving my hands about that. Sorry.
But, you know, one of the new things in this administration is: If you don’t have the answer, don’t guess; just say you don’t know the answer
(Laughter.)
Yeah.
Q Dr. Fauci —
DR. FAUCI: Yes.
Q Dr. Fauci, a couple of questions, if I might. I’d like to follow up with you on what you just said about this strain in South Africa. Has that strain made its way to the United States? And what, if any, concerns do you have? How much do we understand about it?
DR. FAUCI: Great question. Thus far, it does not appear at all that the South African strain is in the United States. However, we must be honest and say that the level of comprehensive sequence surveillance thus far is not at the level that we would have liked. So we’re going to be looking very, very carefully for it. But given the information we have today, it doesn’t appear that the South African strain is here.
Q Okay. And if I could just ask you about the effort to distribute the vaccines, because, of course, that’s what most people want to know: when are they going to get a vaccine. Is the Biden administration starting from scratch with the vaccine distribution effort, or are you picking up where the Trump administration left off?
DR. FAUCI: No, I mean, we certainly are not starting from scratch because there is activity going on in the distribution.
But if you look at the plan that the President has put forth about the things that he’s going to do — namely, get community vaccine centers up, get pharmacies more involved; where appropriate, get the Defense Production Act involved, not only perhaps with getting more vaccine, but even the things you need to get a good vaccine program — for example, needles and syringes that might be more useful in that. So it’s taking what’s gone on, but amplifying it in a big way.
Q President Biden said that what was left was “abysmal,” essentially. Is there anything actionable that you are taking from the previous administration to move it forward?
DR. FAUCI: Well —
Q And is that delaying your efforts to get the vaccine? I mean, that’s the question that —
DR. FAUCI: No, I mean, we’re coming in with fresh ideas, but also some ideas that were not bad ideas with the — with the previous administration. You can’t say it was absolutely not usable at all. So we are continuing, but you’re going to see a real ramping-up of it.
Q One more final question. You had said that most people will be vaccinated by the middle of 2021. Is that still your expectation?
DR. FAUCI: Yes, it is. I mean, I believe that the goal that was set by the President of getting 100 million people vaccinated in the first hundred days is quite a reasonable goal.
And when you get to the point — and one of the things that I think is something we need to pay attention to — and I, quite frankly, have been spending a considerable amount of my own time — is outreaching particularly to minority communities to make sure that you get them to be vaccinated and you explain why it’s so important for themselves, their family, and their community.
If we get 70 to 85 percent of the country vaccinated — let’s say by the end of the summer, middle of the summer — I believe by the time we get to the fall, we will be approaching a degree of normality. It’s not going to be perfectly normal, but one that I think will take a lot of pressure off the American public.
Q Dr. Fauci, you’re one of the few holdovers from the previous administration to this current one. What has been your experience with this new team? And, in your view, what would have been different, in terms of the trajectory of this outbreak from the start, had a team like this been in place at the beginning?
DR. FAUCI: Well, I can tell you my impression of what’s going on right now — the team. I’m — I don’t know if I can extrapolate other things.
But one of the things that was very clear as recently as about 15 minutes ago, when I was with the President, is that one of the things that we’re going to do is to be completely transparent, open, and honest. If things go wrong, not point fingers, but to correct them. And to make everything we do be based on science and evidence.
I mean, that was literally a conversation I had 15 minutes ago with the President, and he has said that multiple times.
Q Is there anything that you, looking back on your comments of the last 10 or 12 months, would like to now, with that sort of license, to amend or clarify?
DR. FAUCI: No. I mean, I always said everything on the ba- — that’s why I got in trouble sometimes. (Laughter.)
Q You mentioned pharmacies. The new CDC director said today that the goal of getting vaccinations into pharmacies by the end of next month isn’t realistic, as had been previously suggested. When will most Americans be able to get a vaccination in their neighborhood pharmacy?
DR. FAUCI: Well, I’m — I didn’t hear that comment. Are you talking about Dr. Welensky’s comment? I didn’t hear that comment, so I don’t really want to comment on the comment. But what she may be saying is that for many people in this country who don’t have access to a pharmacy, they may not be able to utilize getting things in the pharmacy.
I — I’m not sure; I want to be careful because I’m not sure that’s what she said.
We just had a conversation about how we’re going to get vaccines to people who are in pharmacy-desert areas, where they don’t have easy access to a pharmacy. And that’s something we’re working on and taking very seriously.
Q But just to be clear: If you are in an area where you do have access to a CVS or a Walgreens —
DR. FAUCI: Right.
Q — when will you be able to get access to this vaccine —
DR. FAUCI: You know —
Q — like you would a flu vaccine?
DR. FAUCI: You know, in the spirit of not guessing, I really — I’m not quite sure when that will be, but we can get back to you on that.
Q And just on the broader timeline: You mentioned the fall. We just heard the President say, you know, the brutal truth is that it is going to be several more months. Just to be clear, you’re saying by the fall, the majority of Americans —
DR. FAUCI: No.
Q — you think will be vaccinated?
DR. FAUCI: No, I didn’t say that. I said if we get the majority of Americans — 70 to 85 percent — vaccinated by then, we could have a degree of herd immunity that would get us back to normal.
The concern I have, and something we’re working on, is getting people who have vaccine hesitancy, who don’t want to get vaccinated — because many people are skeptical about that. So we really need to do a lot of good outreach for that.
I mean, I don’t know what the best case — the best case scenario, if it were for me, is that we’d get 85 percent of the people vaccinated by the end of the summer. If we do, then by the time we get to the fall, I think we can approach a degree of normality.
Q Dr. Fauci, on the mutations that you were talking about, a question about how exactly they increase transmissibility. Does it take less exposure time to get it? Or does it —
DR. FAUCI: No, no. What it is is that you can do in vitro in a test tube setting, binding an affinity to the receptors, which you have in your nose, in your lung, in your GI tract. The receptor for the virus is called an “ACE2 receptor.” And the facility or affinity with which a virus binds to that means that it very likely will have a better efficiency of infection and replicate more in the nasopharynx. So that’s how you make that determination in the test tube.
Then you look epidemiologically, and you’ll see a spike — going up in the sense of number of cases — and they sort of match each other. A virus that has the ability to easily bind to and replicate with your receptors is one that likely will spread easier.
Q So it doesn’t mean that you’d have more viral load. You —
DR. FAUCI: Well, you could. Yes. In fact, it would mean — because if it binds more easily, it could replicate in the nasopharynx more easily, and it is likely that you would have a higher viral load.
Q So does it make masks less effective in that case?
DR. FAUCI: No, it makes it the reason why you absolutely should be wearing a mask. It doesn’t necessarily make it less effective. If you properly wear a mask, then you’ll be okay.
Q And then, on the UK strain, do you have any data on how widespread that strain is in the United States?
DR. FAUCI: Well, I think it’s in at least 20 states that people have mentioned. Exactly — the real question that’s going to be asked: Is it going to become the dominant strain, or will the strains we already have prevented from flourishing and being the more dominant strain? But it is here, for sure.
Yeah.
Q Just a follow-up on vaccines. Some state and local authorities are saying that they would be able to distribute more vaccines if they had more. Is the Biden administration now trying to increase production by Moderna and Pfizer in the next six weeks?
DR. FAUCI: Yeah, as well as to utilize what we hope will be another player in the field: the J&J, Janssen, as well as other of the companies. But also, as the — as the President has said in his plan, to do whatever he can to expand the availability of vaccines, whatever that is. I mean, he said that he’s going to just use every possibility, including the Defense Production Act.
Q And can you explain the discrepancy between what some states are saying about needing more vaccines and the CDC saying that a lot of vaccine is still remaining on people’s — or on their shelves?
DR. FAUCI: Yeah, you know, I think that that is something that we need to really take a close look at because that is sort of an inconsistent discrepancy, and one of the things we want to do is to find out why that’s the case. And if it is the case — particularly the thing that would be most disturbing: if there’s vaccine laying around, and people are not using it when others would need it.
But I don’t know the answer to that question, but we need to look into it.
Q Dr. Fauci, you’ve joked a couple times today already about the difference that you feel in being kind of the spokesperson for this issue in this administration versus the previous one. Can you — can you talk a little bit about how free, how much different — do you feel less constrained?
What is the — you know, I mean, you — for so many times, you stood up behind the podium with Donald Trump standing behind you. That was a different — that was a different feeling, I’m sure, than it is today. Can you talk a little bit about how you feel kind of released from what you had been doing for the last year?
DR. FAUCI: Yeah, but you said I was joking about it. I was very serious — (laughs) — about it. I wasn’t joking.
No, actually, I mean — I mean, obviously, I don’t want to be going back, you know, over history, but it was very clear that there were things that were said — be it regarding things like hydroxychloroquine and other things like that — that really was uncomfortable because they were not based on scientific fact.
I can tell you I take no pleasure at all in being in a situation of contradicting the President, so it was really something that you didn’t feel that you could actually say something and there wouldn’t be any repercussions about it.
The idea that you can get up here and talk about what you know, what the evidence, what the science is, and know that’s it — let the science speak — it is somewhat of a liberating feeling.
Q I mean, you were basically banished for a few months there for a while. (Laughter.) Do you feel like you’re back now?
DR. FAUCI: I think so. (Laughter.)
Okay.
MS. PSAKI: Well, that’s Mike Shear, if you don’t want to take questions from him in the future. (Laughter.)
Thank you, Dr. Fauci, so much for joining us. We really appreciate it, and we’ll have him back again.
DR. FAUCI: Thank you.
Source: WhiteHouse.gov