So you’ve gotten your coronavirus vaccine, waited the two weeks for your immune system to respond to the shot and are now fully vaccinated. Does this mean you can make your way through the world like the old days without fear of spreading the virus?
Does Vaccination Completely Prevent Infection?
The short answer is no. You can still get infected after you’ve been vaccinated. But your chances of getting seriously ill are almost zero.
Many people think vaccines work like a shield, blocking a virus from infecting cells altogether. But in most cases, a person who gets vaccinated is protected from disease, not necessarily infection.
Every person’s immune system is a little different, so when a vaccine is 95% effective, that just means 95% of people who receive the vaccine won’t get sick. These people could be completely protected from infection, or they could be getting infected but remain asymptomatic because their immune system eliminates the virus very quickly. The remaining 5% of vaccinated people can become infected and get sick, but are extremely unlikely to be hospitalized.
Vaccination doesn’t 100% prevent you from getting infected, but in all cases it gives your immune system a huge leg up on the coronavirus. Whatever your outcome – whether complete protection from infection or some level of disease – you will be better off after encountering the virus than if you hadn’t been vaccinated.
Does Infection Always Mean Transmission?
Transmission happens when enough viral particles from an infected person get into the body of an uninfected person. In theory, anyone infected with the coronavirus could potentially transmit it. But a vaccine will reduce the chance of this happening.
In general, if vaccination doesn’t completely prevent infection, it will significantly reduce the amount of virus coming out of your nose and mouth – a process called shedding – and shorten the time that you shed the virus. This is a big deal. A person who sheds less virus is less likely to transmit it to someone else.
This seems to be the case with coronavirus vaccines. In a recent preprint study which has yet to be peer reviewed, Israeli researchers tested 2,897 vaccinated people for signs of coronavirus infection. Most had no detectable virus, but people who were infected had one-quarter the amount of virus in their bodies as unvaccinated people tested at similar times post-infection.
Less coronavirus virus means less chance of spreading it, and if the amount of virus in your body is low enough, the probability of transmitting it may reach almost zero. However, researchers don’t yet know where that cutoff is for the coronavirus, and since the vaccines don’t provide 100% protection from infection, the Centers for Disease Control and Prevention recommends that people continue to wear masks and social distance even after they’ve been vaccinated.
What About the New Coronavirus Variants?
New variants of coronavirus have emerged in recent months, and recent studies show that vaccines are less effective against certain ones, like the B1351 variant first identified in South Africa.
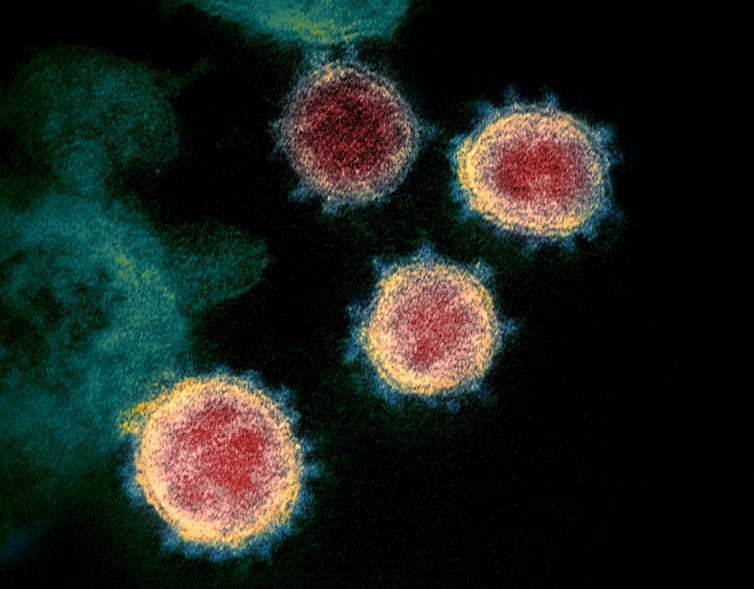
Every time SARS-CoV-2 replicates, it gets new mutations. In recent months, researchers have found new variants that are more infective – meaning a person needs to breathe in less virus to become infected – and other variants that are more transmissible – meaning they increase the amount of virus a person sheds. And researchers have also found at least one new variant that seems to be better at evading the immune system, according to early data.
So how does this relate to vaccines and transmission?
For the South Africa variant, vaccines still provide greater than 85% protection from getting severely ill with COVID–19. But when you count mild and moderate cases, they provide, at best, only about 50%-60% protection. That means at least 40% of vaccinated people will still have a strong enough infection – and enough virus in their body – to cause at least moderate disease.
If vaccinated people have more virus in their bodies and it takes less of that virus to infect another person, there will be higher probability a vaccinated person could transmit these new strains of the coronavirus.
If all goes well, vaccines will very soon reduce the rate of severe disease and death worldwide. To be sure, any vaccine that reduces disease severity is also, at the population level, reducing the amount of virus being shed overall. But because of the emergence of new variants, vaccinated people still have the potential to shed and spread the coronavirus to other people, vaccinated or otherwise. This means it will likely take much longer for vaccines to reduce transmission and for populations to reach herd immunity than if these new variants had never emerged. Exactly how long that will take is a balance between how effective vaccines are against emerging strains and how transmissible and infectious these new strains are.
ABOUT THE AUTHOR
Deborah Fuller is a Professor of Microbiology, School of Medicine, University of Washington. Fuller investigates new vaccine and antiviral concepts aimed at achieving broader, more universal protection against a wider range of highly variable viruses. Toward this goal, the Fuller Lab has designed a therapeutic HIV DNA vaccine that when administered in combination with antiretroviral drugs to nonhuman primates infected with a primary isolate of SIV, induces profound control of viral replication that persists after antivirals are withdrawn. Viral control in this model correlated with strong mucosal CD8 responses localized in the gut, and this finding has more recently led us to investigate new DNA vaccine approaches that can more precisely focus CD8 against highly conserved epitopes and novel genetic adjuvants that can localize these responses to the gut, which is a primary source of residual virus. Similarly, using DNA and RNA vaccines and antivirals designed to precisely target highly conserved regions in influenza, we have shown significant protection against a wide range of influenza strains in mice, ferrets and nonhuman primates. More recently, we have shown that DNA and RNA vaccines can be rapidly developed in response to an emerging pandemic such as COVID-19. These studies demonstrate the feasibility of these new platforms for achieving broad protection against HIV and influenza and as a rapid response to emerging pandemics.. Studies currently in progress in the Fuller lab aim to elucidate mechanisms of protection mediated by these strategies and investigate various approach including novel adjuvants, DNA and RNA vaccine delivery approaches and combinatorial regimens to further improve these outcomes. Results from their work has resulted in over a dozen patents and two start-up biotechnology companies.
This article is courtesy of The Conversation.


