A new study, conducted on more than 140 samples from 12 infected patients, contributes to a better understanding of the dynamics of disease transmission
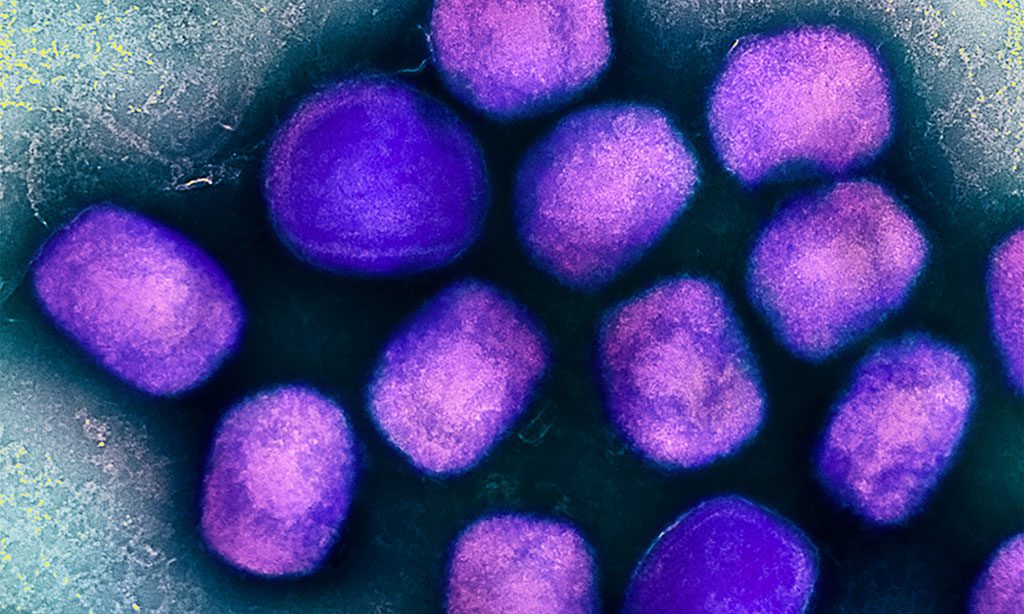
Viral DNA can be frequently detected in different clinical samples from monkeypox-infected patients, including saliva and semen, according to a new study led by the Barcelona Institute for Global Health (ISGlobal).
The study, published in Eurosurveillance, contributes to a better understanding of how this emerging disease is transmitted.
The current monkeypox outbreak represents another zoonotic disease that has crossed borders. In the last six months, more than 9000 cases of monkeypox have been reported worldwide in countries where the disease is not endemic. Initial cases were detected in Britain, Portugal and Spain, mainly in men who have sex with men. However, the disease has spread to many other countries and there is concern that it may spread to vulnerable populations, such as immunocompromised patients or children.
The disease is known to be transmitted by direct contact with the lesions of an infected patient or by surfaces contaminated by these lesions, but little is known about the possible presence of virus in other biological samples , such as saliva, urine or semen.
In this study, the team led by Mikel Martinez , ISGlobal researcher, and Jose Luis Blanco (Hospital Clinic), investigated the presence of genetic material of the virus in different biological samples , collected at different times, from 12 patients with confirmed monkeypox infection . At the time of diagnosis, a high viral DNA load was detected in the skin lesions of all patients. In addition, DNA was detected in the saliva of all cases , some of them with high viral loads . Only one previous study had tested saliva, in one single patient. Viral DNA was also detected in rectal (11 of 12 patients), nasopharyngeal (10/12 patients), semen (7/9 patients), urine (9/12 patients) and faecal (8/12 patients) samples.
“A couple of previous studies had already shown occasional presence of viral DNA in some samples and in some patients, but here we show that viral DNA is frequently present in various biological fluids , particularly saliva, during the acute phase of the disease, and up to 16 days after the onset of symptoms in one patient,” explains Aida Peiró , first author of the study.
The authors point out that the presence of viral DNA does not necessarily mean infectious virus , and that the next step will be to try to isolate infectious virus from such samples. However, the high viral load detected in saliva or semen suggests that such fluids have infectious potential, they add.
“The results of our study contribute to a better understanding of the mechanisms and dynamics of virus transmission , as well as the possible role of sexual transmission ,” Martinez concludes.
Frequent detection of monkeypox virus DNA in saliva, semen, and other clinical samples from 12 patients, Barcelona, Spain, May to June 2022. Eurosurveillance, 14 July 2022.
Read also:
Phylogenomic analysis of the monkeypox virus (MPXV) 2022 outbreak: Emergence of a novel viral lineage? Travel Medicine and Infectious Disease
We performed a phylogenomic analysis of available Monkeypox virus (MPXV) genomes to determine their evolution and diversity. Our analysis revealed that all MPXV genomes grouped into three monophyletic clades: two previously characterized clades and a newly emerging clade harboring genomes from the ongoing 2022 multi-country outbreak with 286 genomes comprising the hMPXV-1A clade and the newly classified lineages: A.1 (n = 6), A.1.1 (n = 1), A.2 (n = 3) and B1 (n = 262), where lineage B.1 includes all MPXV genomes from the 2022 outbreak. It was estimated that B.1 lineage of this clade emerged in Europe on 03/02/2022. The exceptional surge of cases and the broader geographical expansion suggest multifactorial factors as drivers of the current outbreak dynamics. Such factors may include the cessation of smallpox vaccination and its potential spread across particular networks. Integrating pertinent epidemiological information with genomic surveillance information will help generate real-time data to help implement adequate preventive and control measures by optimizing public health decisions to mitigate this outbreak.
Monkeypox outbreak in Madrid (Spain): clinical and virological aspects. Journal of Infection
We extracted data from 48 patients, all cisgender men. The median age was 35 years (IQR 29 – 44), and 87.5% were MSM. The most prevalent symptoms were the presence of vesicular-umbilicated and pseudo-pustular skin lesions (93.8%), asthenia (66.6%), and fever (52.1%). In addition, the location of the lesions in the genital or perianal area was related to the role in sexual intercourse (p<0.001). Sequencing analysis indicated the virus circulating in Spain belongs to the western African clade. Like the other European cases in the outbreak, the Spanish isolates are a direct descendant of viruses previously detected in Nigeria, the UK, Singapore, and Israel in 2017-2018.
Monkeypox infection during pregnancy: European registry to quantify maternal and fetal risks. Ultrasound in Obstetrics & Gynecology
As this neglected virus is spreading in Europe and may represent a threat for pregnant women, it seems paramount to collect and centralize data to quickly quantify the risk associated with exposure during pregnancy. We have therefore adapted our registry for emergency viruses and pregnancy to accommodate monkeypox. A report on maternal and fetal outcomes after exposure during pregnancy showed a 25% risk of severe maternal illness and up to 75% risk of adverse fetal outcome: miscarriage and intrauterine fetal demise with congenital dermal lesions after maternal-fetal transmission. Neonatal demise after a rash potentially related to congenital monkeypox has also been reported. Registry reporting includes variables related to maternal disease, including therapeutic options and neonatal follow-up to document potential skin lesions and well as outcomes follow-up to monitor the safety and effectiveness of monkeypox vaccines during pregnancy.