The United States stands at a dangerous crossroads in biomedical science and public health. A new paper published in JAMA Health Forum warns that proposed cuts to the National Institutes of Health (NIH)—now exceeding 40% for fiscal year 2026 under the Trump administration’s budget—could do lasting damage to the nation’s scientific infrastructure, economy, and preparedness for future health crises.
The analysis uses systems modeling to trace how these funding cuts could unravel the interconnected mechanisms that sustain America’s biomedical innovation engine. The findings are unambiguous: far from saving money, NIH budget reductions could unleash a cascade of consequences that increase healthcare costs, weaken the scientific workforce, and compromise national health security.
These are not speculative risks—they are systemic vulnerabilities, already beginning to materialize. Hundreds of grants have been canceled. New project approvals have plummeted by half. The scaffolding of U.S. biomedical research is being dismantled in real time.
Foundational Science at Risk
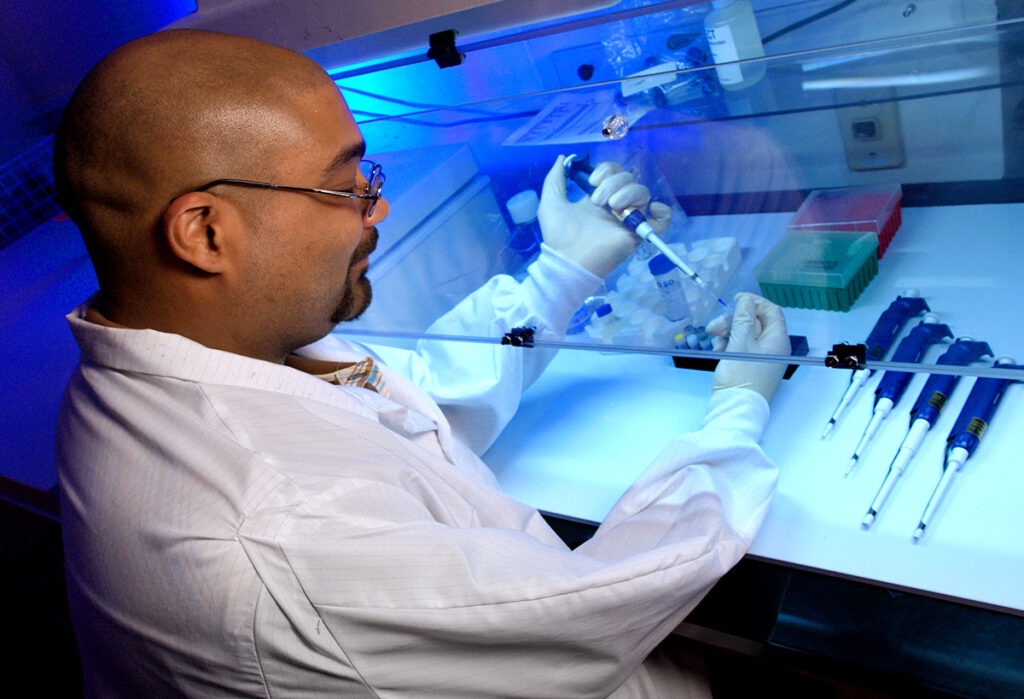
NIH is the backbone of biomedical discovery in the United States. It funds over 50,000 competitive research grants, supports training programs at more than 2,500 institutions, and seeds innovations that private industry later brings to market. The new analysis outlines how slashing NIH funding initiates a “fundamental research contraction loop”—a feedback cycle in which the depletion of public investment starves the pipeline of breakthrough discoveries.
Many of the therapies and technologies that define modern medicine—from cancer immunotherapies to mRNA vaccines—originated in NIH-funded basic science. Without that early-stage research, such breakthroughs would have been delayed, diminished, or abandoned altogether. Industry cannot and does not fill this gap; high-risk, long-horizon research lacks the short-term returns that markets demand.
With fewer NIH dollars, these critical projects won’t be postponed—they’ll be erased.
Scientific Workforce Collapse Is Already Underway
Perhaps even more alarming is the threat to the U.S. biomedical workforce. The study identifies a reinforcing “human capital erosion” loop, wherein reduced funding for training and salaries drives researchers out of the field, decimates lab capacity, and reduces institutional viability.
The numbers are stark. In previously documented funding gaps, labs lost 40% of their personnel and saw publication output drop by 90%. Nationally, NIH investment supports over 400,000 jobs and generates nearly $95 billion in economic activity each year. Gutting this infrastructure doesn’t just cost jobs—it hemorrhages talent that cannot be easily rebuilt.
Once dismantled, scientific capacity—labs, mentors, intellectual networks—takes years or decades to recover, if at all.
“Without careful consideration of these dynamics, efforts to reduce federal spending could ultimately erode the very systems that make the US a global leader in scientific breakthroughs and undermine opportunities for long-term cost savings in health care.”
— Jalali & Hasgul, JAMA Health Forum (2025)
Private Sector Won’t Save Us—and May Make It Worse
Some policymakers argue the private sector will pick up the slack. The study dismantles this myth. As public funding recedes, private research will likely pivot further toward high-revenue therapies, leaving population-scale needs like prevention, early detection, and non-commercial diseases behind.
This market tilt is already well documented in areas like antibiotic resistance and Alzheimer’s, where major pharmaceutical companies have withdrawn due to profitability concerns. The result? Fewer tools to fight global health threats and higher prices for treatments that do reach the market.
This shift feeds another destructive loop: the “rising cost of new treatments,” which inflates healthcare spending and places added strain on public systems—ironically intensifying the budget pressures that prompted NIH cuts in the first place.
Prevention Efforts Slashed, Future Crises Magnified
NIH doesn’t just fund innovation—it helps prevent illness at scale. The paper outlines how budget cuts compromise public health interventions that improve life expectancy and reduce long-term care costs. Investments in cancer screening, climate-health research, vaccine confidence, and pandemic preparedness are being rolled back or canceled entirely.
The consequences will not be immediate, but they will be devastating. Delayed diagnostics, stalled translational research, and unpreparedness for emerging threats all drive up morbidity, mortality, and medical costs. This is the “lost savings from prevention” loop: by defunding upstream solutions, we all pay more downstream—in dollars and lives.
A National Security Threat in Plain Sight
Beyond the spreadsheets and budget lines, this is a national security issue. The U.S. biomedical research complex is as strategically vital as any defense system. NIH-backed science enabled America’s rapid COVID-19 vaccine response and underpins biodefense, cancer detection, and antimicrobial resistance preparedness. Gutting this capability weakens national resilience and cedes ground to global competitors.
Other countries are increasing public research investments to attract top talent and lead the next generation of science. The U.S., meanwhile, is slashing its own future. If this trajectory holds, it will mark a historic reversal in global scientific leadership.
The Bottom Line for Policymakers and the Public
The authors of the paper do not offer partisan arguments—they map systemic consequences. Their model is a warning system, not a prediction. But the feedback loops they describe are already activating.
For public health leaders, academic institutions, and life science companies, the implications are clear: this is not an abstract policy debate—it is an unfolding structural crisis. If federal support for biomedical research collapses, rebuilding it will be slow, costly, and potentially impossible in key areas.
As the U.S. considers its budget priorities, it must recognize that NIH funding is not a discretionary luxury—it is a foundational investment in health, innovation, and national strength. Cuts made today will cost far more tomorrow—in money, talent, and human life.
Jalali MS, Hasgul Z. Potential Trade-Offs of Proposed Cuts to the US National Institutes of Health. JAMA Health Forum, 25 July 2025.