A Rising Tide of Cholera and a Strain on Response
Cholera, a centuries-old disease that thrives where clean water and sanitation are scarce, is again testing the world’s capacity to manage preventable epidemics. The World Health Organization’s Multi-country Cholera Situation Report No. 30 (26 Sept 2025) underscores the persistence and complexity of this crisis: from January to August 2025, 462,890 cases and 5,869 deaths were reported across 32 countries, with the African and Eastern Mediterranean Regions bearing the heaviest toll.
While the number of cases has fluctuated month to month, the rise in fatalities—up 118 percent compared with the same period in 2024—signals deeper systemic weaknesses. Limited healthcare access, climate shocks, and conflict-driven displacement are amplifying the disease’s reach. The WHO classifies the global risk level as very high, emphasizing that these figures almost certainly underestimate the true burden due to underreporting in conflict zones and disaster-hit areas.
Modeling the Epidemic: What Science Reveals
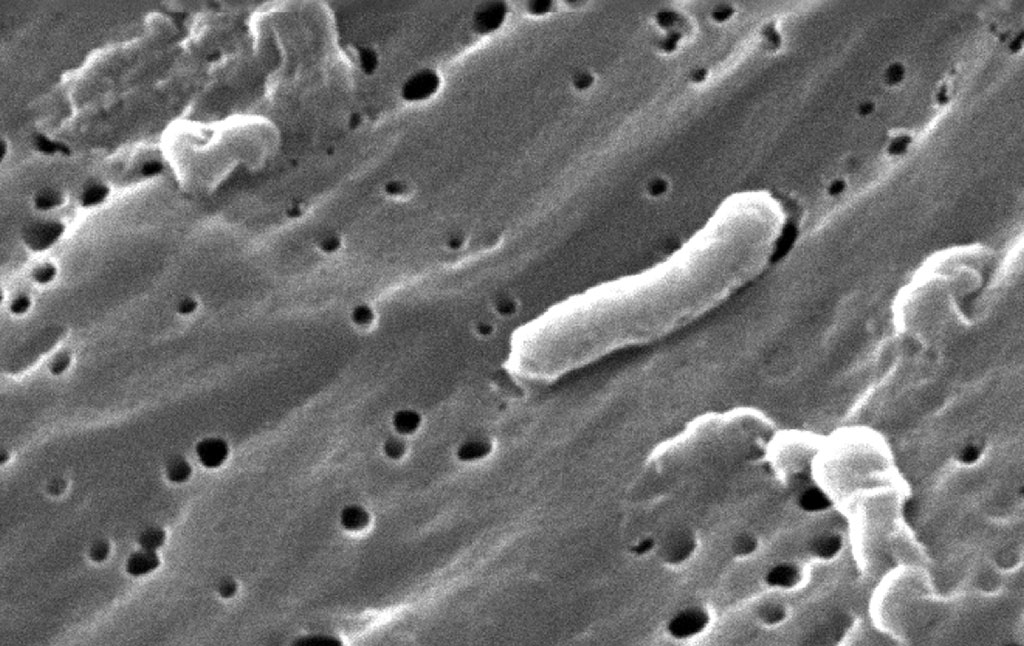
A new BMC Public Health study provides a rigorous analytical complement to WHO’s surveillance data. Using a mathematical and machine-learning model to assess outbreaks in eight African countries, the researchers estimate a median basic reproduction number (R₀) of 2.0, with values reaching as high as 2.8 in Mozambique—meaning that, without intervention, each case can lead to roughly two more.
The modeling highlights key drivers: waterborne transmission, inadequate sanitation, bacterial shedding from untreated cases, and the compounding influence of extreme weather events. Importantly, it identifies how timely intervention—through vaccination, hygiene measures, and safe-water access—can substantially reduce spread. Countries such as Malawi, which sustained robust WASH and surveillance initiatives, saw measurable declines in 2023 despite regional pressures.
Early Action Pays Off: Lessons from the DRC
In the Democratic Republic of the Congo, where cholera remains endemic, a novel anticipatory action framework is demonstrating the benefits of acting before crisis peaks. A joint effort by OCHA, WHO, UNICEF, and the DRC’s national cholera program linked real-time local surveillance with pre-authorized humanitarian financing from the UN Central Emergency Response Fund (CERF).
When thresholds were triggered in 2023, CERF released $750,000 within days—funds that enabled partners to reach more than 230,000 people with chlorinated water, sanitation facilities, and 18 new treatment centers. The result: a case fatality rate of just 0.27 percent, well below the 1 percent global benchmark. The pilot was expanded in 2025, proving that early, data-triggered responses save lives and reduce costs.
When Global Aid Withers: The U.S. Funding Freeze
Yet, even as science and innovation advance, global financing for cholera control has faltered. According to an October 2025 analysis by the Center for Global Development (CGD), the U.S.—historically the largest humanitarian donor—implemented a sweeping aid freeze in early 2025. The freeze suspended most USAID awards and shuttered the agency, nominally exempting “lifesaving” programs but excluding preventive measures such as WASH and reproductive health services.
CGD’s data, combining Africa CDC epidemic reports with U.S. spending data, reveal a troubling correlation: as U.S. WASH disbursements declined, cholera mortality in Africa surged, with Angola, the DRC, Sudan, and South Sudan alone accounting for more than 3,000 deaths by mid-2025. Although some funding has since resumed, few new humanitarian awards have been issued—a gap that undermines prevention and rapid response efforts precisely when global vaccine stocks remain below emergency levels.
Why This Matters: Cholera and Health Security
Cholera’s resurgence is not merely a humanitarian failure—it is a health-security concern. The same conditions that fuel its spread—poor sanitation, population displacement, and fragile infrastructure—also facilitate outbreaks of other water- and vector-borne pathogens. As the world learned from COVID-19 and Ebola, the destabilization of basic public-health systems in one region can rapidly echo across borders. Investing in cholera prevention—clean water systems, surveillance, and rapid-response funding—is, therefore, not charity but a strategic imperative for global and national stability.
The Path Forward
The converging evidence from WHO, CGD, and recent scientific studies points to clear priorities:
- Expand anticipatory and locally triggered financing mechanisms that release funds before outbreaks escalate.
- Rebuild and sustain international aid commitments, particularly for WASH and vaccine supply chains.
- Integrate modeling and real-time data into national cholera control programs to better predict and contain transmission.
- Protect public-health infrastructure as a pillar of global security—because diseases that thrive on neglect ultimately test the resilience of all nations.
Sources and Further Reading:
World Health Organization: Multi-country outbreak of cholera: External Situation Report No. 30
BMC Public Health: Understanding cholera dynamics in African countries with persistent outbreaks
Center for Global Development: Cholera in Africa: Rising Deaths, Shrinking U.S. Aid
PreventionWeb / Centre for Humanitarian Data: How anticipatory action in the DRC is saving lives from cholera