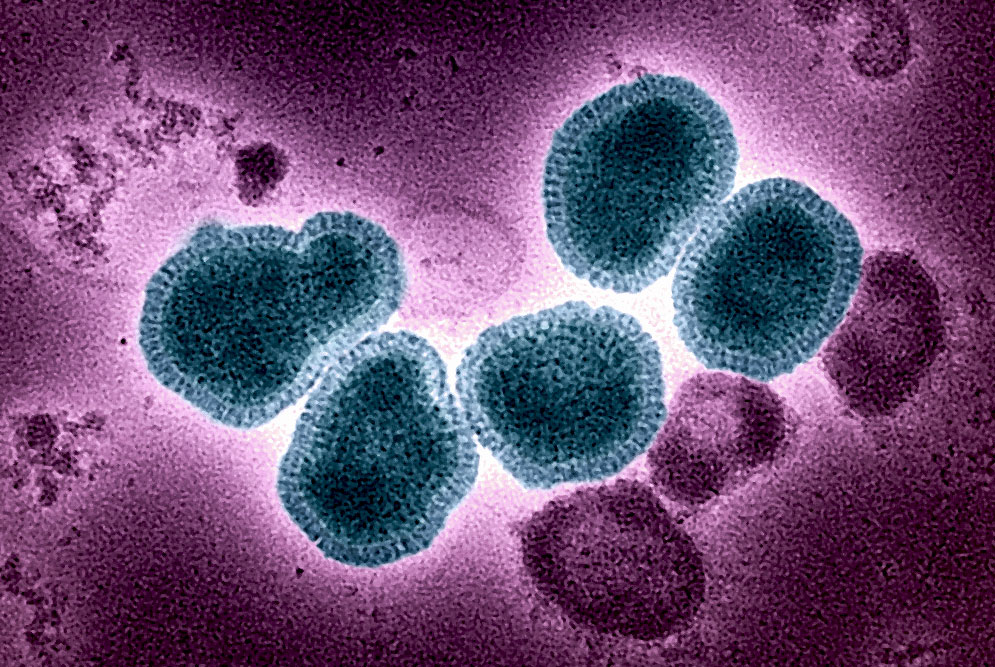
The 2024–25 influenza season in the United States has been classified as one of the most severe in recent history, with hospitalization rates surpassing all seasons since at least 2010. The findings, published in the Morbidity and Mortality Weekly Report by the U.S. Centers for Disease Control and Prevention (CDC), underscore the impact of co-circulating influenza A(H1N1)pdm09 and A(H3N2) viruses and raise fresh concerns about vaccination uptake and antiviral use.
Record-High Hospitalizations
Between October 2024 and April 2025, more than 38,000 laboratory-confirmed influenza hospitalizations were reported through the Influenza Hospitalization Surveillance Network, which covers roughly 9% of the U.S. population. The cumulative hospitalization rate reached 127.1 per 100,000 people—nearly double the historical median of 62.0. This was not only the highest rate recorded since systematic monitoring began in 2010, but it also exceeded hospitalization peaks from severe respiratory virus surges such as COVID-19 Omicron waves.
Older adults bore the greatest burden. Those aged 75 and older experienced a rate of nearly 600 hospitalizations per 100,000, while children aged 5–17 recorded the lowest rate at 39.3. Still, across all age groups, hospitalization rates were 1.8 to 2.8 times higher than typical seasonal levels.
Virus Dynamics and Age-Specific Risks
The season was characterized by simultaneous circulation of two major influenza A subtypes. Patients with A(H1N1)pdm09 infection faced higher hospitalization rates (72.2 per 100,000) than those with A(H3N2) (49.5). Interestingly, among adults over 75, A(H1N1) hospitalizations were more common than A(H3N2), reversing a pattern seen in prior high-severity seasons such as 2017–18, when A(H3N2) predominated.
CDC researchers suggest that birth cohort immunity may have influenced outcomes. Older adults retain partial protection from earlier exposures to H1-type viruses, making them more vulnerable in seasons dominated by H3N2. The 2024–25 co-circulation pattern may have shifted hospitalization risk across age brackets.
Vaccination and Treatment Gaps
Vaccination coverage among hospitalized patients remained low. Only about one-third (32.4%) had received the influenza vaccine prior to admission. Nearly 29% of cases had missing vaccination data, reflecting ongoing challenges in timely reporting.
Encouragingly, most hospitalized patients (84.8%) received antiviral treatment, but significant disparities emerged by age. Adolescents aged 5–17 years were least likely to be treated (61.6%), while treatment rates exceeded 88% among the oldest adults. Given the well-documented benefits of early antiviral use in reducing complications and deaths, this treatment gap represents an urgent area for intervention.
Severe Clinical Outcomes
Despite record-high hospitalizations, the severity of individual cases remained in line with past seasons. Nearly 17% of patients required intensive care, 6% needed invasive mechanical ventilation, and 3% died while hospitalized. Pneumonia, sepsis, and acute renal failure were among the most frequent complications. Importantly, 11% of hospitalized patients had no underlying medical conditions, highlighting that otherwise healthy individuals are not immune to the consequences of severe influenza.
Challenges Ahead
The extraordinary burden of influenza during the 2024–25 season raises questions about preparedness for future high-severity years. Declining vaccination rates in the general population may have amplified the impact of circulating viruses. With influenza hospitalizations surpassing even those of COVID-19 and RSV this season, public health leaders stress the need for renewed investment in prevention strategies.
The CDC continues to recommend annual influenza vaccination for everyone aged six months and older, coupled with prompt initiation of antivirals for all hospitalized patients. As influenza patterns remain unpredictable, strengthening vaccination campaigns, improving antiviral use in children and adolescents, and maintaining readiness for surges in hospital demand will be essential for mitigating future seasons of high severity.
O’Halloran A, Habeck JW, Gilmer M, et al. Influenza-Associated Hospitalizations During a High Severity Season — Influenza Hospitalization Surveillance Network, United States, 2024–25 Influenza Season. MMWR Morbidity and Mortality Weekly Report, 11 September 2025.
Related Reading:
The Pediatric Infectious Disease Journal: Disease Burden of the 2024–2025 Influenza Season in Children
U.S. Medicine: Veterans’ Flu Cases, Severity Exceeded COVID-19 Last Flu Season
U.S. Centers for Disease Control and Prevention: FluSight 2024-2025 Evaluation