In 2016, an estimated 90,000 people died from measles – an 84% drop from more than 550,000 deaths in 2000, according to the World Health Organization.
From The Shadow Crusade to End Measles by Maryn McKenna (Wired):
After the thrill of eradicating smallpox, declared gone from the world in 1980 after a 14-year effort, global health planners dreamed big dreams about the other diseases they would vanquish. But in the years since, eradication efforts stalled. The campaign against Guinea worm has been going since 1980; polio, since 1988; river blindness, in the Americas, since 1992.
Smallpox had been chosen not just because it was a killer, but because it possessed qualities that made eradication plausible. It affected only humans and couldn’t hide in animals or the environment. It produced visible signs of illness, quickly—epidemiologists could easily trace who had infected whom—and its symptoms were unique. And it could be prevented with just one dose of a vaccine.
As it happens, measles fits those conditions too—more so than the other diseases that have been in public health’s sights since. It has no nonhuman host. It can be detected with a reliable diagnostic test. And it can be prevented with a single vaccine dose (though kids in the United States get two childhood doses, just to be sure).
A dark gift of eradication campaigns is that their intense focus on a disease reveals things that research had never recognized before. It wasn’t until the polio campaign began that vaccine-derived polio was even discovered. Years down the line, scientists have realized the mutated virus can be a long-lasting risk. It can reproduce for years in the guts of people with certain immune system disorders, making them permanent emitters of infectious virus that passes into sewage. That’s driven development of new antiviral drugs to give to those long-term excreters, to prevent them from being the disease’s last refuge.
Through nationwide use of vaccination, endemic measles (i.e., a transmission chain lasting 12 months or longer) was eliminated in the United States in 2000. Yet, importations of measles from endemic countries continue to occur, leading to outbreaks. From 2001 to 2015, the overall annual incidence of measles remained extremely low (less than 1 case/million population) compared with incidence worldwide (40 cases/million population); relative increases in measles rates were observed over the period, and the findings suggest that failure to vaccinate may be the main driver of measles transmission, according to a study published by JAMA.
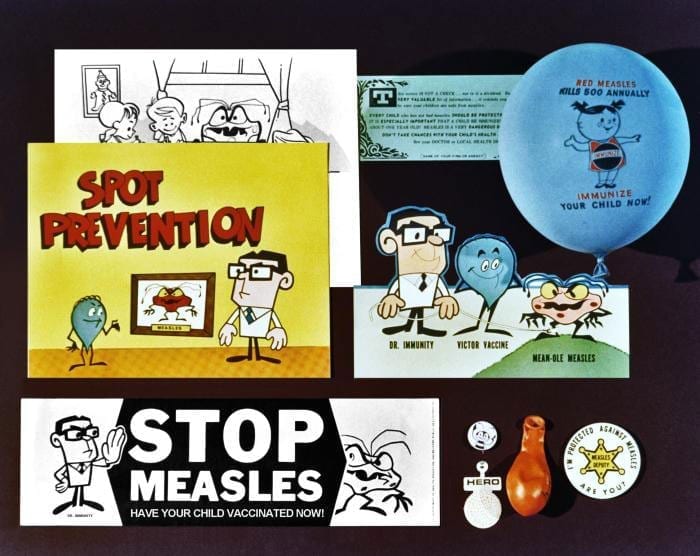
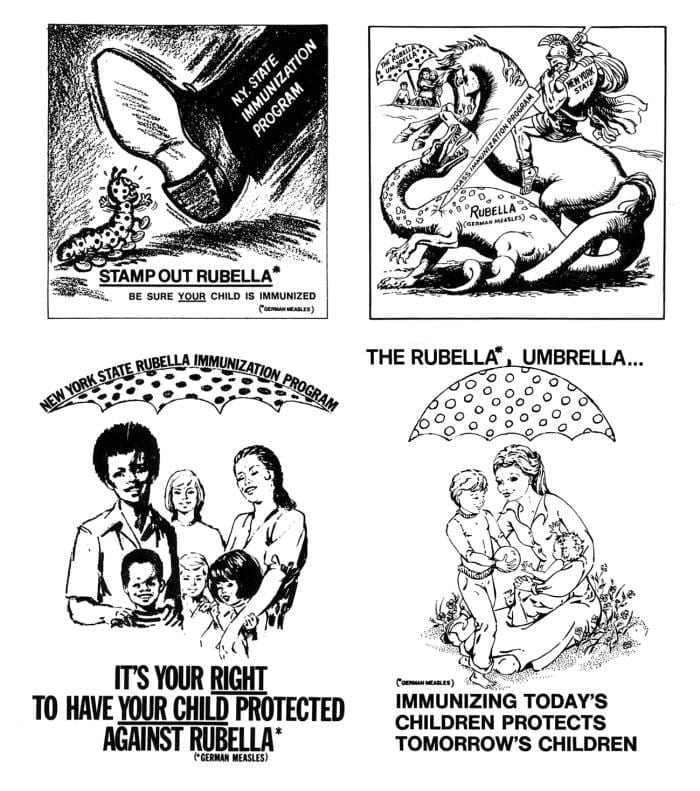
But in an era of vaccine hesitancy and misinformation, even small reductions in childhood measles vaccinations in the U.S. would produce disproportionately large increases in the number of measles cases and in related public health costs. A 5 percent drop in the number of children ages 2 to 11 inoculated against the measles, mumps and rubella would potentially triple the number of annual measles cases in this age group.
The additional measles cases would increase annual public health expenditures by at least $2.1 million, or $20,000 per case of measles, according to the CDC.

Related Resources:



