From working to develop one of the first nonhuman primate models for the 2019 novel coronavirus disease (COVID-19) to designing new therapeutic strategies and nanotechnology-based tests to rapidly diagnose infections, researchers at Tulane University are responding across disciplines to the emerging coronavirus epidemic.
Tulane National Primate Research Center (TNPRC) is establishing a COVID-19 research program to develop a vaccine and test treatments against the virus. First, researchers will create a nonhuman primate model to study the disease’s clinical progression, how it is transmitted through the air and how it specifically affects aging populations. Investigators hope to answer many of the unknowns about the disease, including why older individuals are more susceptible to complications and death from it.
Earlier this year, TNPRC mobilized to become one of the first research facilities in the country to obtain approval from the Centers for Disease Control to receive samples of the novel coronavirus, called SARS-CoV-2. TNPRC is the only National Primate Research Center with a Regional Biocontainment Laboratory (RBL) onsite that is capable of the high level of biocontainment required to study an emerging infectious disease like COVID-19. It also has the nation’s largest capacity for studying the transmission of infectious agents in nonhuman primates at this level of biocontainment, which is critical as public health responders rush to understand and thwart disease spread.
COVID-19 is caused by a virus called SARS-CoV-2. The virus is a member of the coronavirus family that is a close cousin to the SARS and MERS viruses that have caused outbreaks in the past. There have been more than 75,000 confirmed cases and at least 2,000 deaths from the virus, according to recent figures from the World Health Organization (WHO). While most of the cases are in China, the outbreak has spread to 25 countries with 15 confirmed cases in the United States. The virus likely evolved from animal hosts to one that can spread from person to person.
TNPRC will use a grant from the Brown Foundation to collect preliminary data as researchers seek federal and philanthropic funding for more expansive coronavirus research efforts.
“The goal of this technology is to aim for earliest disease detection, to provide better predictors of disease progression, rapid differentiation of coronavirus species, and real-time monitoring of how patients respond to treatments so we can improve outcome. This is especially urgent now since there have been reports that COVID-19 is spreading prior to people knowing that they are sick.”
Tony Hu, PhD, Weatherhead Presidential Chair in Biotechnology Innovation
Rappaport will lead a team of collaborators from the center with unique expertise in aerobiology, virology, immunology, pulmonology, and veterinary medicine. All work will be conducted in the RBL under the highest, most stringent safety and quality standards and overseen by Tulane Director of Biosafety Angela Birnbaum, a nationally certified biosafety expert.
Birnbaum leads a national working group that will launch a collaborative research program on COVID-19 among the National Primate Research Centers (NPRCs). The group will work to develop vaccines and evaluate treatments against the disease using a nonhuman primate model. It will release research findings to scientists and collaborators in real time to accelerate progress to find successful treatments and preventions against the disease.
“To respond effectively to a global outbreak that is moving as quickly as this, it is essential to have collaboration and data sharing between the NPRCs to help inform the public health response,” Birnbaum said. “And it’s imperative that this work is done with the strictest safety protocols in place as we learn more about this pathogen.”
Tulane researchers will also work to develop a rapid test for COVID-19 using advanced diagnostics developed by Tony Hu, PhD, Weatherhead Presidential Chair in Biotechnology Innovation. Hu will lead the project which will use highly sensitive blood or saliva tests that rely on nanotechnology-based strategies to find biomarkers of disease. Researchers at the Center of Cellular and Molecular Diagnosis of the Tulane School of Medicine will work with investigators at the TNPRC to validate the tests using the nonhuman primate model.
Tulane math professor leads effort to map spread of coronavirus
Other researchers across Tulane are working on COVID-19 efforts. Virologist Bob Garry is part of a team decoding the genome of the coronavirus to determine its origins and how it possibly evolved from bats and pangolins. Epidemiologist and disease ecologist Lina Moses, PhD, at Tulane School of Public Health and Tropical Medicine is in Geneva coordinating research efforts with WHO and the Global Outbreak Alert and Response Network as they work to prevent the outbreak from spreading into a global epidemic.
Leading disease modeling expert James “Mac” Hyman in Tulane School of Science and Engineering is creating mathematical models to track the spread of the coronavirus and the effectiveness of efforts to stop it.
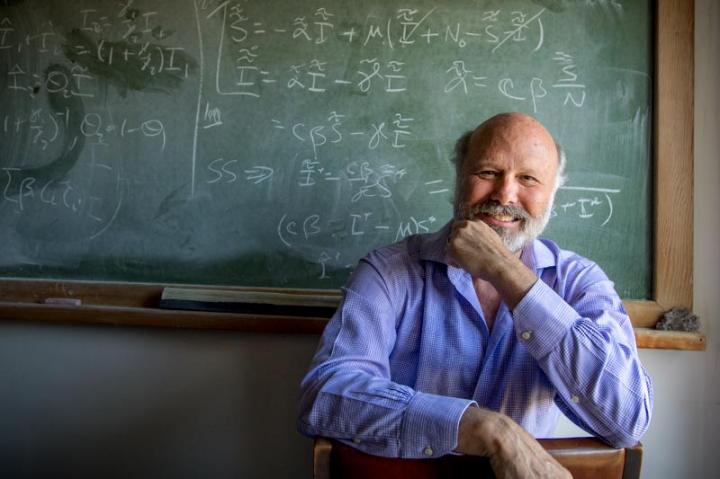
Credit: Paula Burch-Celentano
Hyman and colleagues at Georgia State University and the Public Health Agency of Canada recently had a paper on COVID-19 accepted by the journals Infectious Disease Modeling and the Journal of Clinical Medicine.
The paper is based on daily reported cases of the virus for each Chinese province from the National Health Commission of China. The paper provides a methodology to predict the number of new infections five, 10, and 15 days in the future for the current epidemic in China.
In the paper, the authors say the predictions can help public health officials prepare the medical care and allocate resources needed to confront the epidemic, as well as to predict the intensity and type of interventions needed to mitigate an epidemic. In the absence of vaccines or antiviral drugs for the virus, the effective implementation of non-drug interventions, such as personal protection and social distancing, will be critical to bringing the epidemic under control.
“We’re trying to create models that can be more effective in guiding public health efforts to mitigate an epidemic,” Hyman said. “It’s about figuring out what needs to be in a model to estimate the risk of someone being infected and predict the risk that an infected person will be to someone else.
“In the coronavirus, we must account for the way that an infected person can infect the environment, such as a table or door handle, and others can be infected, even if they don’t have direct contact with an infected person.”
In a note submitted to Science Translational Medicine, Hyman and colleagues said several groups are working independently to predict the spread of COVID-19 and that coordination among the groups is essential and should be supported by government agencies.
He thinks the World Health Organization needs to take the lead by organizing an international effort that focuses on three specific aims – predicting further spread of the virus in China, predicting its potential to spread elsewhere or under various conditions, and predicting the effectiveness of mitigation strategies, such as quarantine, contact reduction, hand hygiene and face masks.
“In the complex ‘fog of an outbreak,’ the world needs actions guided by expert consensus and, as emphasized in this editorial, further guided by data-driven models that explore response scenarios,” he wrote.


