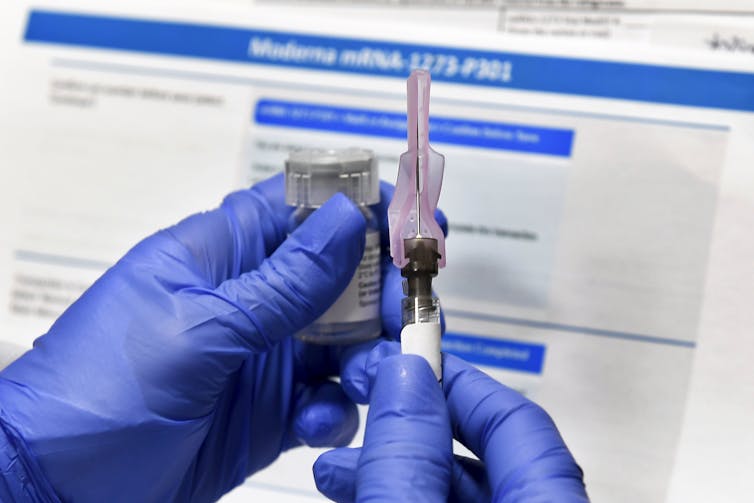
Just like a fresh piece of fish, vaccines are highly perishable products and must be kept at very cold, specific temperatures. The majority of COVID-19 vaccines under development – like the Moderna and Pfizer vaccines – are new RNA-based vaccines. If they get too warm or too cold they spoil. And, just like fish, a spoiled vaccine must be thrown away.
So how do companies and public health agencies get vaccines to the people who need them?
The answer is something called the vaccine cold chain – a supply chain that can keep vaccines in tightly controlled temperatures from the moment they are made to the moment that they are administered to a person.
Ultimately, hundreds of millions of people in the U.S. and billions globally are going to need a coronavirus vaccine – and potentially two doses of it. This mass vaccination effort is going to require a complex vaccine cold chain on a scale like never before. The current vaccine cold chain is not up to the task, and expanding the supply chain is not going to be easy.
Cold chain problems mean wasted vaccines
Most vaccines need to be stored within 1 degree Fahrenheit of their ideal temperature. Traditional vaccines are usually stored between 35 degrees Fahrenheit and 46 degrees Fahrenheit, but some of the leading COVID-19 vaccines need to be stored at much colder temperatures. Moderna’s vaccine requires a storage temperature of minus 4 degrees Fahrenheit, whereas Pfizer’s vaccine candidate requires a storage temperature of minus 94 degrees Fahrenheit. These are not easy temperatures to maintain accurately.
A study from 2019 estimated that 25% of vaccines are degraded by the time they arrive at their destination. If a vaccine is exposed to temperatures outside its range, and this gets noticed, then the vaccines are always thrown away. Rarely, a temperature mistake is missed and one of these vaccines is administered. Research shows that these vaccines won’t cause any adverse effects, but could offer decreased protection and might require a patient to be revaccinated.
Temperature mistakes are mostly due to inappropriate shipping procedures in the cold chain, and these losses are estimated at US$34.1 billion annually. But that number does not even take into account the cost – physically as well as financially – of any illnesses that could have been prevented by timely deliveries of high-quality vaccines.
As a scholar of operations management, I study perishable product supply chains in the pharmaceutical industry and how they relate to product quality. With billions of vaccines needed to address the pandemic, a high spoilage rate would result in an immense financial loss and a huge delay in vaccinations that could result in deaths and a longer global shutdown.

The cold chain today
Experts estimate that somewhere between 12 billion and 15 billion COVID-19 vaccines are needed globally.
Currently, the world is capable of producing and distributing around 6.4 billion flu vaccines per year. In 2021, experts expect companies will produce around 9 billion COVID-19 vaccines, and the cold chain must be able to handle this huge increase on top of the vaccines that must be distributed every year already.
The cold chain requires three major pieces of infrastructure: planes, trucks and cold storage warehouses. How the infrastructure is connected and utilized depends on the vaccine production locations and the points of demand.
Once a COVID-19 vaccine is produced, it likely will be immediately transported by truck to the nearest suitable airport. Since a COVID-19 vaccine is particularly valuable and time sensitive, it will likely be shipped via air transport across the country or world. After these planes are unloaded, the vaccines will be taken via truck to appropriate warehouse storage facilities for transportation to distribution facilities. Some of the vaccines may be directly shipped from the warehouses to health care facilities where the vaccinations will take place.
Preparations and solutions
So what can companies, health agencies and governments do to help expand the cold chain?
The first step will be to identify where the vaccines will be produced. If production is done mainly abroad, companies will need to use trucks and planes for transportation within their own countries and for further distribution to others.
There is also a lot of uncertainty about which COVID-19 vaccine will be approved first. Different vaccines may require different temperatures and different handling procedures. Hence, staff throughout the cold chain would need different training on how to handle each vaccine.
Another question is how frequently deliveries will need to be made to points of care. This will depend on the refrigeration capacity of health care organizations and hospitals, staffing resources, the locations the vaccines will be given and many other factors, including the shelf life of the vaccine itself.

Finally, there is the simple problem of how to expand shipping and storage capacity.
Typical restaurant freezers have a range of 5 degrees Fahrenheit to minus 10 degrees Fahrenheit and simply can’t reach the temperatures required by something like the Pfizer vaccine. Specialized equipment is needed.
Several major logistics companies, including UPS and DHL, are already investing in new storage facilities for cold chain management. UPS is adding freezer farms of 600 freezers capable of reaching minus 80 degrees Celsius near UPS air hubs in Louisville, Kentucky, and the Netherlands. Each freezer will be able to hold 48,000 vials of vaccine and could easily store either the Pfizer vaccine or the Moderna vaccine at the necessary low temperatures.
Installing freezers capable of the low temperatures needed by the Pfizer vaccine isn’t possible in many places, so it is essential that processes be put into place to make sure those areas can receive a steady supply of the vaccine.
Airports and logistics companies are currently evaluating whether they can meet this need. The results remain to be seen.
These are just a few of the major problems and potential solutions, but there are dozens of interesting scenarios that could arise.
For example, if the U.S. government gets involved in distribution, there is a possibility that the military would transport vaccines. Constant electricity becomes essential as well. In regions where fire risk is leading to blackouts or in developing nations where the grid is not as reliable, thousands of vaccines could be lost if the power goes out. It is also expected that only certain airports certified for handling pharmaceuticals will be able to accept such valuable, perishable cargo, so bottlenecks may occur there. And finally, it’s possible that with the airline companies reeling from the pandemic, there might not be enough active planes to meet the demand for shipping these vaccines.
Every vaccine produced could save a life and bring the world closer to a return to normalcy, but getting the vaccines to where they need to be is not going to be easy. Preparing and fortifying the cold chain for vaccine distribution will ensure that vaccines are not wasted and will help the world get through this pandemic sooner.
ABOUT THE AUTHOR
Anna Nagurney is the John F. Smith Memorial Professor of Operations Management and the Director of the Virtual Center for Supernetworks at the Isenberg School of Management at the University of Massachusetts Amherst. Dr. Smith has published over 200 journal articles and 14 books on various network themes including supply chains. Recent awards include being elected a Fellow of the Network Science Society in 2019 and receipt of The Constantin Carathedory Prize from the International Society of Global Optimization. In 2020 she received the Harold Larnder Prize.
This article is courtesy of The Conversation.



