When the efficacy of the Oxford/AstraZeneca vaccine was announced in late 2020, there was some confusion. The overall efficacy of the vaccine at stopping people developing symptomatic COVID-19, two weeks after the second dose, was 70%. But this wasn’t the whole picture.
This figure was based on averaging the results from two groups. In one group, which was given two full doses, the vaccine was 62% effective at stopping people developing symptoms. But in the second group, a dosing error meant that volunteers received a half dose followed by a full one. This ended up being 90% protective against developing COVID-19.
This was intriguing. Why would giving people less of the vaccine lead to a more effective immune response? The answer to this may lie in the design of the vaccine, and could mean that there are ways to make this vaccine – and others that use the same design – more effective.
How the Oxford Vaccine Works
Vaccines work by exposing the immune system to recognisable parts – or “antigens” – of pathogens that cause disease, such as bacteria or viruses. The immune system then mounts a response. Immune cells called B cells make antibodies to destroy the pathogen. Sometimes T cells can also be called into action, which eliminate our own cells that have been infected with the pathogen.
Some B and T cells then remember the antigens for the future. At some future point, if the person is exposed to the pathogen, these long-lasting memory cells can quickly order more antibodies to be made to destroy the pathogen and attack infected cells.
In effect, the principle of vaccination is to “mimic” an infection, but in a controlled way so that immunity is generated without causing illness. After a few weeks, once T cells and B cells have been generated, the person vaccinated will be protected. For certain vaccines, this requires two doses, as in some people the first dose alone won’t generate complete immunity. The booster dose ensures as many people as possible acquire protection.
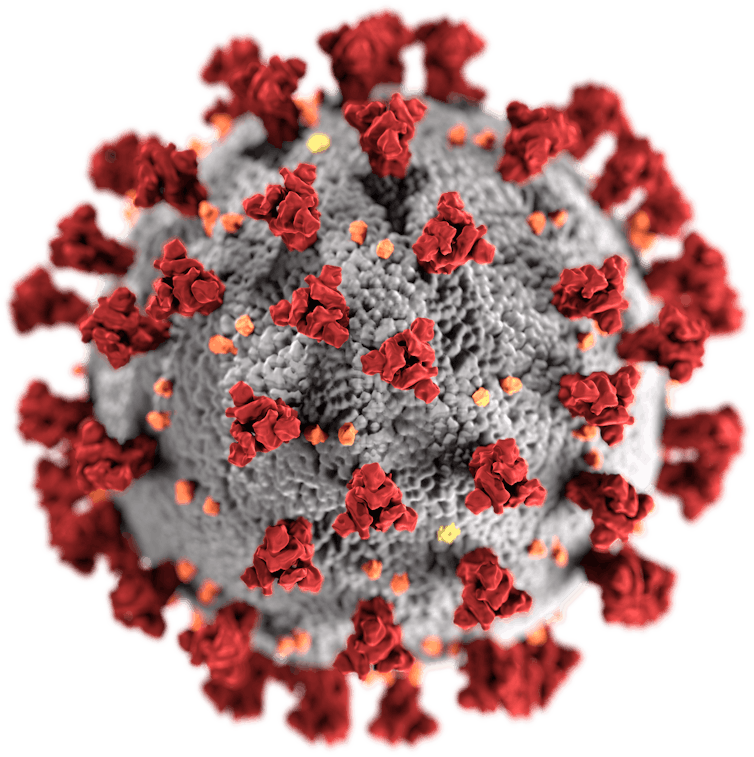
In the case of the coronavirus vaccines, a number of methods are used to present the virus’s antigens to the immune system. Some, such as the Sinopharm and Sinovac vaccines in China, simply present the body with a whole, inactivated version of the coronavirus. But others instead instruct the vaccinated person’s own cells to produce a specific part of the coronavirus: the spike protein on its outer surface, which is a particularly recognisable antigen.
These vaccines do this by delivering the part of the coronavirus’s genetic code that encodes the spike protein into the cells of the body, which then read the code and start making the protein. Some, such as the Pfizer/BioNTech and Moderna vaccines, deliver the code in the form of messenger RNA (mRNA). Others use a harmless virus to get the genetic code inside cells; the Oxford vaccine uses chimpanzee adenovirus, genetically altered so that it’s unable to reproduce, called ChAdOx1. These are known as viral-vector vaccines.
How Design Could Affect Efficacy
It’s not yet known why the reduced-dose regimen of the Oxford vaccine showed better efficacy in trials, but it could be down to the viral vector.
When a person is given a viral-vector vaccine, as well as generating an immune response against the coronavirus’s spike protein, the immune system will also mount a response against the viral vector itself. This immune response may then destroy some of the booster dose when it is subsequently delivered, before it can have an effect. This has long been recognised as a problem.
However, a lower first dose might not allow for a strong anti-vector immune response to develop, which could leave the booster dose unscathed and lead to greater overall efficacy. If it turns out that this is the case, then future work will need to establish the optimum dosing regimen for generating the strongest immune response.
The Russian Sputnik V vaccine acknowledges that immunity to the viral vector could be a problem, but comes up with a different solution. It uses two different human adenoviruses – Ad26 and Ad5 (out of the 50 that affect humans) – for its two vaccine doses. This heterologous (or hybrid) vaccine, with different vectors for prime and booster vaccinations, is less likely to have one jab generate an immune response against the viral vector that then interferes with the other. The vaccine is therefore less likely to have a reduced efficacy.
The Gamaleya Center, the lab that made Sputnik V, said that after two doses the efficacy of the vaccine is over 90% (though it has yet to publish full results demonstrating this). This has now led to AstraZeneca testing a new hybrid vaccine schedule, comprising one dose of its vaccine and one of the Ad26-vector Sputnik V, to see if this makes the Oxford/AstraZeneca vaccine more effective.
ABOUT THE AUTHOR
Jameel Inal is a Professor of Immunobiology, London Metropolitan University, and Visiting Professor of Biomedical Science, University of Hertfordshire. After a degree in Microbiology from King’s College London and MPhil in the molecular biology of Bacillus thuringiensis and the use of natural gene transfer systems, Jameel then worked in vaccine development for his PhD, at the Centre for Applied Microbiology and Research at Porton Down (this was part of the Public Health Laboratory Service, now the Health Protection Agency). During this time he also gained experience of working with ACDP category 3 pathogens. He had two W.H.O. fellowships in the Immunology Unit, at the Dept. of Medical Parasitology at the London School of Hygiene and Tropical Medicine, continuing his work in vaccinology, applied to the human Schistosoma parasite. He then worked for one year as a Research Assistant at the Ludwig Institute for Cancer Research (UCL-Middlesex branch), working in the lab of Prof. Mike Waterfield on PI3 kinase signalling. During his second period at LSHTM he discovered a new complement regulatory protein receptor in the Schistosoma parasite and went on with funding from the Sir Halley Stewart Trust to characterise this together with Prof. Bob Sim at the MRC Immunochemistry Unit, Univ. of Oxford. From 2000, he continued for the next five years his research in complement regulation as a Senior Research Fellow, at the University Hospital Basel, Switzerland, in the Dept. of Biomedicine. With funding from the Research Foundations of Roche and Novartis and capital venture funding, his team, with help from Innogenetics NV in Belgium, developed a synthetic peptide, able to therapeutically inhibit complement-mediated inflammation in vivo. In 2005 Jameel returned to London, as a Senior Lecturer at London Met. Two years on he was made Professor of Immunology. In late 2007 he started his first experiments on microvesicles, from a preliminary interest in their ability to inhibit complement activation. In January 2009 he founded the Cellular and Molecular Immunology Research Centre, or CMIRC and became a founding member of the International Society for Extracellular Vesicles. He is on the editorial panel of Scientific Reports and has been on the editorial panel of the Journal of Extracellular Vesicles. He also hosted ‘Microvesiculation and Disease,’ the second such meeting in the UK, in September 2012. Since 2010, Jameel has published 39 papers and one book chapter in this new field. In December 2017 Jameel moved as the Professor of Biomedical Science to the School of Life and Medical Sciences (LMS) at the University of Hertfordshire to head the Biosciences Research Group. From November 2018 he was Associate Dean for Research in LMS and as of May 2020 has taken the role of Visiting Professor in Biomedical Science, whilst taking on the role of Professor of Immunobiology at London met. He has supervised 13 PhDs to completion and his main research focus is on Extracellular Vesicles in infectious disease and cancer.
This article is courtesy of The Conversation.



