A new study published in the journal Ethics, Medicine and Public Health by researchers from the University of Rome Tor Vergata examines the growing intersection of Ebola virus disease (EVD), biological warfare (BW), and public health preparedness. Conducted as part of the International Master Courses in Protection Against CBRNe Events, this scoping review outlines how Ebola’s lethality, infectiousness, and global spread potential make it a viable candidate for weaponization—and why existing CBRNe (Chemical, Biological, Radiological, Nuclear, and Explosive) defense frameworks must be adapted to address this complex threat.
This research arrives amid increasing concern about the dual-use nature of virology, where scientific advances intended for human health can be repurposed for destructive purposes. By analyzing outbreaks, technical vulnerabilities, and emergency response data, the authors highlight the urgent need for international collaboration, integrated biosecurity policy, and sustained investment in health infrastructure to confront the evolving landscape of biothreats.
Ebola: From Natural Threat to Weaponization Risk
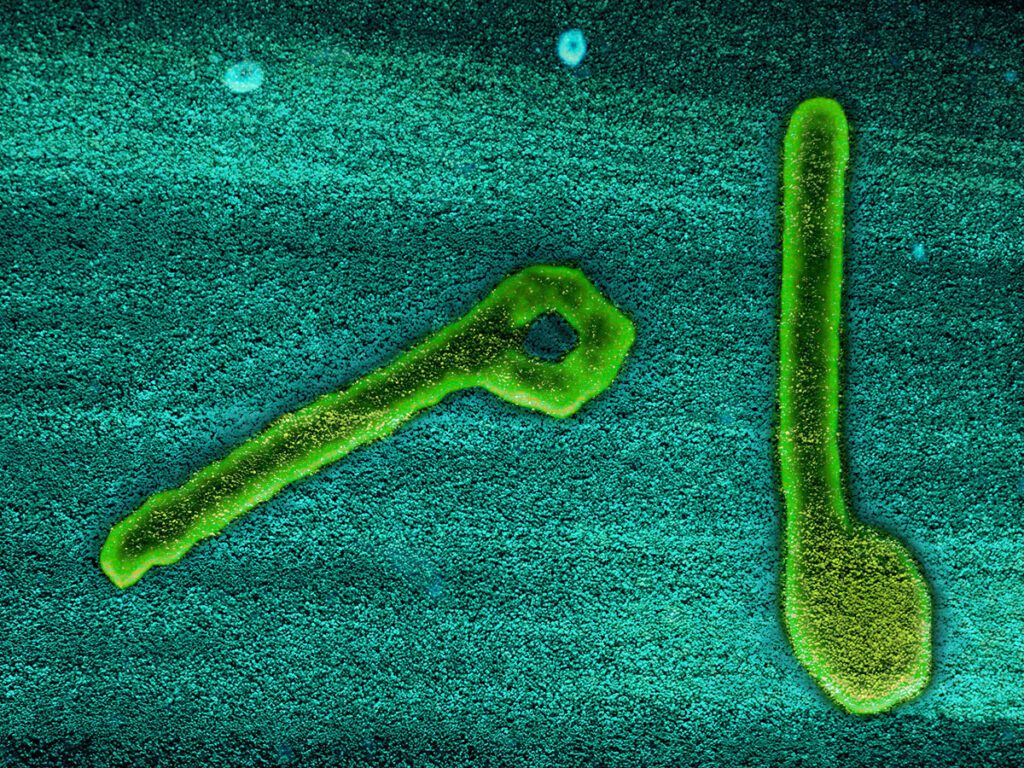
Ebola virus disease is widely recognized for its rapid onset, high mortality, and devastating impact in outbreak settings. But the virus’s pathogenic characteristics—combined with limited therapeutic options—also place it at the center of discussions about biological weapons.
The authors emphasize that while weaponizing Ebola requires advanced biosafety containment and genetic engineering capabilities, it remains a viable concern. Historical efforts such as those by the Japanese Aum Shinrikyo cult and former Soviet bioweapons programs highlight that interest in filoviruses as biological agents is not merely theoretical.
Of growing concern is the risk of “low-tech” bioterrorism, in which infected individuals might be used as vectors, spreading the virus intentionally through global travel systems or densely populated areas. This bypasses the need for sophisticated delivery systems and puts pressure on public health surveillance networks to detect and contain outbreaks at their source.
CBRNe Strategies Offer a Blueprint for Resilience
The review proposes the CBRNe approach as a critical framework to strengthen biodefense against high-consequence pathogens like Ebola. CBRNe protocols integrate early warning surveillance, rapid diagnostics, PPE deployment, decontamination, and interagency coordination—tools essential for managing both natural and deliberate outbreaks.
One of the study’s central insights is that Ebola-specific adaptations of CBRNe strategies are essential. Unlike spore-forming bacterial threats (e.g., anthrax), Ebola requires more intense fluid-containment measures, longer quarantine duration, and real-time diagnostic capabilities in austere environments.
Case studies from Uganda and the Democratic Republic of the Congo (DRC) illustrate the real-world application of these principles, from drone-enabled PPE deliveries to the deployment of portable sequencing labs in conflict zones. These examples highlight the benefits—and challenges—of implementing high-standard CBRNe procedures in settings with limited infrastructure.
Global Health and National Security Intertwined
Why does this matter beyond defense policy circles? The risk of Ebola’s use in a bioterrorist attack extends far beyond borders—it directly threatens global health security. As the West African outbreak of 2014–2016 showed, Ebola’s rapid transmission and disruption of healthcare systems can destabilize economies, overwhelm medical infrastructure, and spark mass fear.
In an age of globalized travel and interconnected economies, the intentional misuse of a virus like Ebola could cripple public services, disrupt trade, and ignite geopolitical tensions. For the U.S. and other nations, investing in public health preparedness is not just a moral imperative—it is a matter of national security and economic resilience. The review authors call for stronger integration between civilian public health systems and national biodefense initiatives to ensure a coordinated response to biological crises, regardless of their origin.
Bridging the Gaps: Technology, Ethics, and Equity
The researchers also raise critical ethical considerations regarding access to diagnostic technologies, the potential for surveillance overreach, and the equitable distribution of countermeasures like vaccines and PPE. While developed countries increasingly invest in high-tech bio-surveillance and stockpile experimental treatments, many Ebola-endemic nations lack even basic diagnostic infrastructure.
This imbalance poses not just a humanitarian concern but a strategic vulnerability. A delay in detecting or containing an Ebola outbreak—whether natural or intentional—in one region can become a global emergency in days. The authors advocate for tiered preparedness models, affordable diagnostics, and policy reforms to prevent the militarization of public health without undermining civil liberties or trust.
Looking Forward: A Roadmap for Integrated Preparedness
The paper concludes that Ebola exemplifies a broader trend: the blurring lines between naturally occurring epidemics and potential acts of bioterrorism. The CBRNe framework, when tailored to the nuances of EVD, offers a pathway for integrating defense-grade preparedness with public health priorities.
To operationalize these recommendations, the study urges training of multidisciplinary response teams, clearer coordination protocols between military and civilian actors, and equitable investment in global surveillance infrastructure. The challenge is formidable—but the cost of inaction could be catastrophic.
Ludovici GM, Tassi PA, Iannotti A, Russo C, Quaranta R, Manenti G, Malizia A. Bioterrorism and CBRNe threats: The role of Ebola in global security. Ethics, Medicine and Public Health. University of Rome Tor Vergata, June 2025.