In three new studies in the current issue of the International Journal of Infectious Disease, researchers reported on clinical outcomes in Saudi Arabia, how long patients will shed virus during their infections, and how the Oman is dealing with cases that have appeared there.
An editorial in the same issue discusses how the relatively high percentage of MERS-CoV infections have been hospital-acquired, which reduces the possibility that the coronavirus will reach pandemic or even epidemic status.
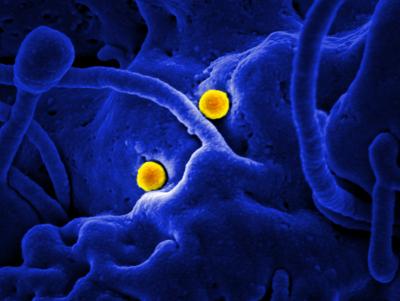
Middle East respiratory syndrome coronavirus (MERS-CoV) is an emerging virus, with the first case reported in 2012. It exhibits a 40% fatality rate and over 97% of the cases have occurred in the Middle East.
Hospital Exposure to Infection
In one study that reports on 70 consecutive cases in Saudi Arabia between October 1, 2012 and May 31, 2014, researchers from Prince Sultan Military Medical City, King Saud University and Al-Faisal University, Riyadh, Kingdom of Saudi Arabia, found a 60% mortality rate. Mortality was only correlated to patients over the age of 65, who were almost 4.5 times more likely to die.
Patients for whom data were collected were mostly of older age (median 62 years), male (65.7%), and had healthcare acquisition of infection (55.7%). Their symptoms included fever (61.4%), dyspnea (60%), and cough (54.3%).The majority developed pneumonia (90%) and required intensive care (70%). Independent risk factors for severe infection requiring intensive care included concomitant infections.
This research team notes that although healthcare exposure to infection was the most important risk factor for the development of MERS-CoV infection, in the ICU setting, where more strict infection control measures were applied, only one healthcare worker acquired the infection and no patient-to-patient transmission occurred.
One of the co-investigators, Professor Ziad A. Memish, MD, Ministry of Health & College of Medicine, Al-Faisal University, Riyadh, Kingdom of Saudi Arabia, comments, “These findings highlight the importance of applying infection control measures in healthcare facilities where patients with suspected MERS-CoV infection are admitted.”
Length of Virus Shedding
In a second study researchers from Alfaisal University, Riyadh, Kingdom of Saudi Arabia, the Ministry of Health, Riyadh, Kingdom of Saudi Arabia, Johns Hopkins Aramco Healthcare, Dhahran, Kingdom of Saudi Arabia, and the Indiana University School of Medicine, Indianapolis, IN, USA, also led by Dr. Memish, analyzed samples from 26 individuals (13 patients and 13 contacts), finding that virus shedding continued for a significant time.
Although contacts cleared more quickly than patients, at 12 days, 76% of cases and 30% of contacts were still positive for MERS-CoV by PCR testing.
Dr. Memish observes that “This finding, if confirmed by the prospective systematic collection of respiratory samples, would highlight the importance of applying prolonged infection control measures in severely ill patients with MERS-CoV in the healthcare setting.”
MERS-CoV in Oman
Since about 22 countries worldwide have reported infection with MERS-CoV, many governments have instituted preparedness plans to deal with possible outbreaks. In a contribution from the Department of Communicable Disease, Ministry of Health; the Department of Child Health, Royal Hospital; the Central Public Health Laboratory, Ministry of Health; and the Department of Infection Prevention and Control, Nizwa General Hospital, all in Oman, researchers present the details of the only two confirmed MERS-CoV cases in Oman to date.
They then describe the key factors of the response plan, public health surveillance and contact management, building laboratory capacity, infection prevention and control, case management, and risk communication.
“Strengthened infection control practices and having a powerful active surveillance program for acute respiratory illnesses are key to the rapid and prompt response for emerging respiratory infections,” cautions lead author I.S. Al-Abaidani, MD, Department of Communicable Disease, Ministry of Health, Oman.
HAI Dominate the Epidemiology
Finally, in an accompanying editorial, Eskild Petersen, MD, from the Departments of Infectious Diseases and Clinical Microbiology at Aarhus University Hospital, Aarhus, Denmark, and Editor-in-Chief, International Journal of Infectious Diseases, Marjorie M. Pollack, MD, Deputy Editor, ProMED-mail and Consultant Medical Epidemiologist, New York, NY, USA, and Lawrence C. Madoff, MD, Editor, ProMED-mail and Professor of Medicine, Division of Infectious Diseases and Immunology, University of Massachusetts Medical School Boston, MA, USA, review the current state of MERS-CoV and emphasize that hospital-acquired infections dominate the epidemiology.
The editorial further notes that transmission on commercial aircraft or other public transportation has not been reported, even after an extensive investigation of airline passengers who traveled to the USA with two well-publicized, infected and symptomatic passengers.
According to the editorial, with most infections occurring in hospital settings, “there is a large potential to reduce transmission through early identification of possible MERS-CoV infected patients thereby leading to early isolation of these patients — ideally at the arrival point in the hospital.”