Health care workers must diagnose and isolate Ebola victims at an early stage to have a chance to save them and prevent the virus from spreading. But the most sensitive and quickest diagnostic test produces a small percentage of false negative results that undermine efforts to control the deadly agent.
Case Western Reserve University (CWRU) researchers have been awarded a $100,000 National Science Foundation (NSF) Ebola rapid response grant to develop a method to reduce the risk of the virus going undetected.
Different forms of Ebola virus have killed 25 percent to 90 percent of those who became infected, according to the World Health Organization. The current outbreak has left more than 8,400 dead in Guinea, Liberia and Sierra Leone, according to recent Centers for Disease Control figures.
Among the dead are surgeon Martin Salia, whose family lives in Maryland. After he fell ill in Sierra Leone, an early test for the disease was negative. By the time he was flown to an Omaha, Neb., hospital for treatment in November, he was in advanced stages of the fast-moving disease and died soon after.
“While Ebola is declining in West Africa, there remains a strong risk of outbreaks in the future,” said Nicole Steinmetz, an assistant professor of biomedical engineering at Case Western Reserve University.
With no vaccine or cure on the horizon, the NSF sought proposals that could quickly improve the status quo.
Steinmetz, the principal investigator of the grant and an appointee of the university’s School of Medicine, is not an expert in human viruses, but has extensive experience in manipulating nanoparticle-sized plant viruses for the benefit of human health.
The problem with the current method, called the reverse transcription polymerase chain reaction test, is that there is no reliable control available to ensure the target of the test is not being destroyed during processing.
The test is designed to detect the presence of Ebola ribonucleic acid, RNA, a key component of the virus’ molecular biology. To extract the viral RNA from the tissue for testing, health care workers have to process the tissues, and the target RNA may be destroyed during the harsh conditions of the assay. These processing errors may remain undetected, resulting in a false negative result.
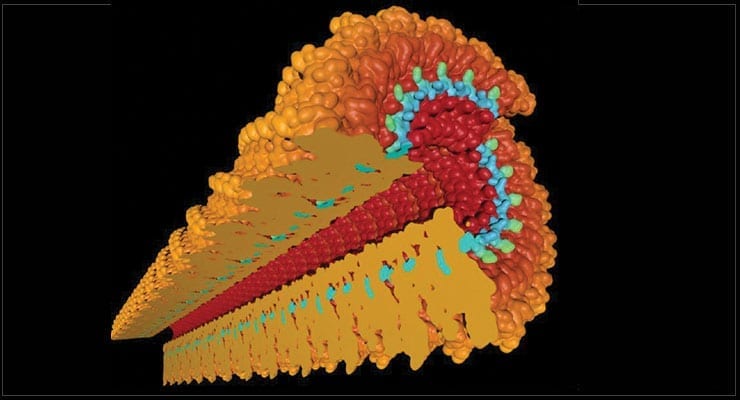
Steinmetz’s lab plans to build a positive control through a bio-inspired nanomanufacturing protocol. The team will make a synthetic, safe form of the Ebola RNA and insert it in a plant virus nanoparticle. The plant virus has a protective protein coat similar to the Ebola virus coat that protects its RNA. This control will mimic Ebola virus realistically and can be added to test samples for detection and monitoring of the processing steps.
The safe RNA will also include a type of marker that can be detected by enzymatic activity, as long as the RNA remains intact. Not detecting the marker at any point would indicate that the processing has degraded the plaint virus RNA and would have also degraded any Ebola virus RNA present, Steinmetz said.
“It tells us a mistake was made and the assay needs to be repeated to rule out a false negative result,” she said. Otherwise, the test could fail to detect the Ebola virus. Therefore, the patient might not be quarantined and treated, and those with whom the patient had close contact would not be tested.
Working with Steinmetz will be Ruth Keri, a professor of pharmacology at the School of Medicine, and the University of Stuttgart’s Christina Wege.
As part of the project, the lab will develop a high-tech test to use in a clinic and a low-tech test for use in the field.
“For the low-tech assay, we’ll need a different process where you don’t have computers or refrigeration,” Steinmetz said. “We hope to develop low-tech kits that can be taken to high-risk areas of Africa and be used to detect the disease earlier rather than waiting on U.S. or European health care workers to fly in and run diagnostics.”
Source: Case Western Reserve University press release, adapted. Image credit: Nicole Steinmetz