A clinical trial evaluating alternative strategies for administering the JYNNEOS monkeypox vaccine to increase the number of available doses has begun enrolling adult volunteers.
Adults ages 18 to 50 years who have not been vaccinated against smallpox or monkeypox previously are eligible to enroll in the NIAID trial. Investigators aim to include a demographically diverse group of volunteers that represents those affected by monkeypox. All trial participants will receive the JYNNEOS vaccine in some form.
The trial, which will enroll more than 200 adults across eight U.S. research sites, is sponsored by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health. JYNNEOS is manufactured by Bavarian Nordic, based in Copenhagen.
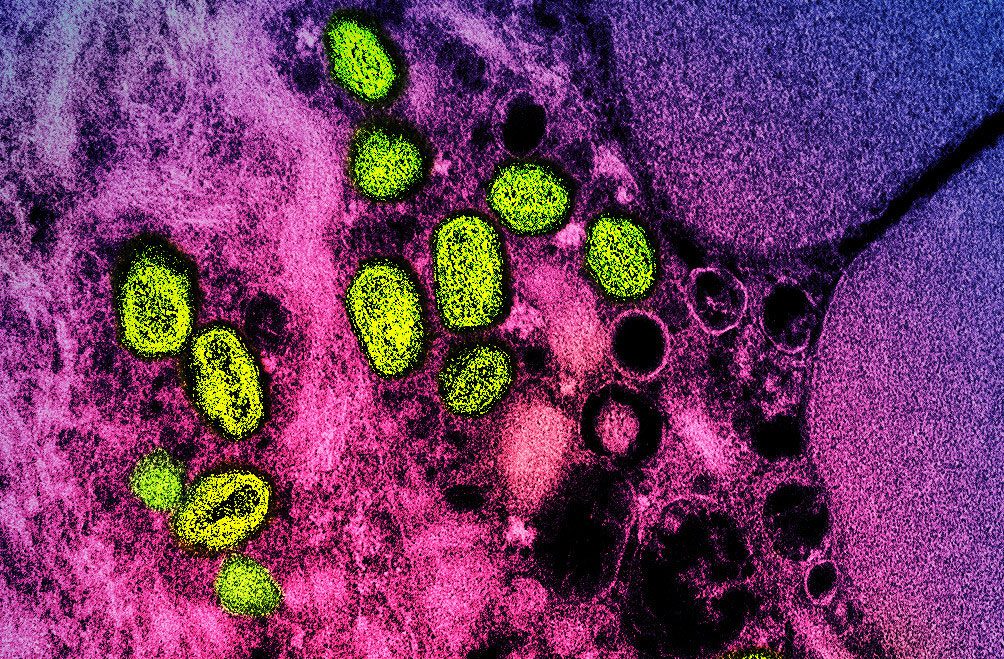
JYNNEOS contains an attenuated orthopoxvirus called modified vaccinia Ankara (MVA), which does not replicate in human cells. It is approved for administration by two subcutaneous (in the tissue beneath the skin) injections 28 days apart; however, the FDA recently authorized intradermal (between layers of the skin) administration of the vaccine for adults, which expands the number of people who can be vaccinated with the currently limited supply. This alternative intradermal dosing regimen uses one-fifth of the standard dose used for subcutaneous administration, allowing health care providers to administer up to five times the number of vaccine doses per vial of JYNNEOS vaccine. NIH-supported researchers demonstrated in a 2015 publication that intradermal administration at one-fifth of the standard dose induced an immune response in recipients that was comparable to the subcutaneous method of administration.
“NIAID’s trial of JYNNEOS will provide important information on the immunogenicity, safety, and tolerability of alternative dosing approaches that would expand the current supply of vaccine, ” said NIAID Director Anthony S. Fauci, M.D.
The Centers for Disease Control and Prevention has reported 20,733 cases of monkeypox in the United States since May 2022. The global outbreak is primarily affecting men who have sex with men. The virus usually causes painful skin lesions and flu-like symptoms. Serious complications—which have been rare in the United States—can include dehydration, bacterial infections, pneumonia, brain inflammation, sepsis, eye infections and death. Historically, the virus is known to be transmitted from person to person through direct contact with skin lesions, body fluids, and respiratory droplets and by indirect contact with items such as contaminated clothing or bedding. Preliminary analyses indicate that sexual transmission may be playing a role in the current outbreak.
Investigators will assess whether the peak immune responses induced in recipients receiving the vaccine intradermally are at least as good as those induced by the licensed subcutaneous regimen and will compare the relative safety and tolerability of the different regimens.
Volunteers will be asked to participate in eight study visits over the course of a year where they will undergo physical examinations and provide blood samples for laboratory evaluations. An independent Data and Safety Monitoring Board (DSMB) will monitor participant safety throughout the duration of the study.
The trial will enroll volunteers at the following sites:
- Saint Louis University in Missouri
- Baylor College of Medicine in Houston
- Brigham and Women’s Hospital in Boston
- The NIH Clinical Center in Bethesda, Maryland
- George Washington University in Washington, D.C.
- Vanderbilt University in Nashville, Tennessee
- The Hope Clinic at Emory University in Decatur, Georgia
- The University of California, San Diego
Investigators anticipate the trial will take 15 months to complete; however, initial results could be available in early 2023.
Trial to Evaluate the Immunogenicity of Dose Reduction Strategies of the MVA-BN Monkeypox Vaccine. ClinicalTrials.gov NCT05512949. This study is a Phase 2 randomized, open-label, non-placebo controlled, multi-site clinical trial that will evaluate two intradermal (ID) regimens for Modified Vaccinia Ankara-Bavarian Nordic (MVA-BN) vaccine compared to the standard subcutaneous (SC) regimen in healthy, vaccinia-naïve adults 18 to 50 years of age, inclusive. At least 210 participants will be enrolled and randomized to one of three study arms. The two dose sparing strategies include one-fifth (2 x 10^7) and one-tenth (1 x 10^7) of the standard dose of MVA-BN administered ID on Day 1 and 29 (Arm 1 and 2, respectively). The comparator arm (Arm 3) will be the 2-dose standard (1 x 10^8) MVA-BN SC regimen.
The primary objectives are: 1) to determine if peak humoral immune responses following an ID regimen of 2 x 10^7 50% Tissue Culture Infectious Dose (TCID50) MVA-BN are non-inferior to the licensed regimen of 1 x 10^8 MVA-BN administered SC; 2) to determine if peak humoral immune responses following an ID regimen of 1 x 10^7 TCID50 MVA-BN are non-inferior to the licensed regimen of 1 x 10^8 MVA-BN administered SC. The secondary objectives are: 1) to determine if individual peak humoral immune responses following each ID regimen are non-inferior to the licensed regimen administered SC; 2) to evaluate humoral immune responses of each ID regimen (separately) compared to licensed SC regimen each study day; 3) to evaluate the kinetics of the humoral immune responses of each ID regimen (separately) compared to licensed SC regimen through Day 365; 4) To compare relative safety among study arms as assessed by systemic and local reactogenicity for 14 days after each vaccination, unsolicited adverse events for 28 days after each vaccination, and serious adverse events (SAE) and medically attended events (MAAE) from Day 1 through Day 57, and related SAE/MAAEs through Day 181.